What Is Osteoporosis?
Overview
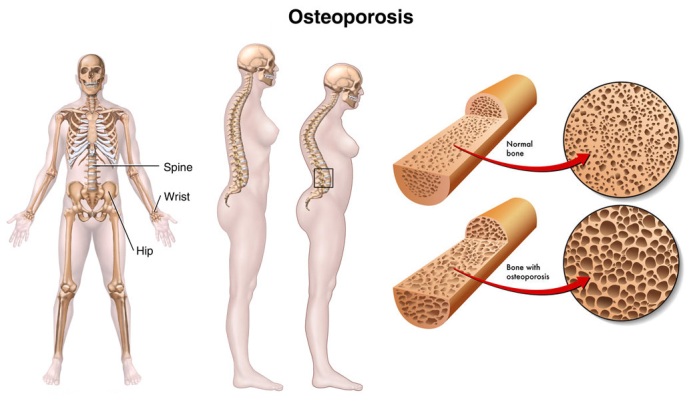
Osteoporosis, which means “porous bones,” is a disease that thins and weakens your bones, making them fragile and more likely to break. It is generally referred to as a “silent disease” as a result of it will develop step by step over a few years while not inflicting any symptoms. You may be able to reduce or delay bone loss and you can treat osteoporosis, but you may not be able to prevent it.
The National Osteoporosis Foundation (NOF) estimates as many as 54 million Americans have osteoporosis and low bone mass. Research shows concerning half ladies and one-quarter of men can break a bone thanks to pathology.
Although men will suffer from pathology, the vast majority of individuals affected by osteoporosis are women. In fact, the annual variety of osteoporotic fractures in ladies is larger than the quantity of heart attacks, strokes and cases of breast cancercombined. Women ar fourfold additional possible to develop pathology than men.
Although the unwellness will strike at any age, women are at greatest risk for osteoporosis after menopause. More than fifty % of non-Hispanic Caucasian and Asian ladies age fifty years and older have low bone mass, increasing their risk for osteoporosis. A major reason for this is often that women’s bodies turn out less estrogenafter biological time, and estrogen plays an important role in helping to prevent bone loss.
Although the common age for biological time within the us is fifty one, some ladies expertise biological time earlier thanks to natural causes or following surgery, illness or treatments that destroy the ovaries. For example, a total hysterectomy in which the ovaries and uterus are removed will immediately trigger menopause. When you haven’t had a catamenial amount for quite twelve consecutive months, while not another medical reason for the absence of your periods, you’re biological time.
The good news is that pathology may be prevented and treated and bone health may be maintained. It is never too late to learn how to maintain and keep your bones healthy.
Bone Basics
Your bones are complex living tissue. They provide structure and support for your muscles, defend your organs and store ninety nine % of the metallic element employed by the soft tissues of your body for his or her numerous functions.
Healthy bone is strong and dense with many interconnecting pieces. Bone full of pathology is porous, fragile and weak.
Bone is formed principally of albuminoid, a macromolecule that has a soft framework, andhydroxyapatite, a complex of calcium and phosphate, minerals that add strength and harden the framework. This combination of albuminoid and metallic element makes bone sturdy nonetheless versatile to face up to stress.
Bone changes often through a method referred to as transforming, during which the body breaks down previous bone and replaces it with new, strong bone. This method continues throughout life, however varies considerably as you age.
From birth to age 25 or 30, the body builds more new bone than it breaks down. By age 30, your bones become the strongest they will ever be. This section of bone development is termed peak bone mass. The level of bone mass achieved at the height is decided mostly by genetic science, however additionally by nutrition, exercise and catamenial perform. Having healthy, strong bones at younger ages can be a critical factor in protecting against osteoporosis in the future.
After concerning age thirty, your body breaks down previous bone quicker than it builds new bone. This process speeds up dramatically as menopause approaches and for several years after. In the initial 5 to seven years following biological time, you can lose up to 20 percent of bone mass.
Bone loss continues at a slower pace throughout the rest of your life and should accelerate once more in your older years, sometimes when age seventy. Rates of bone loss vary among individuals, but even slow rates of loss may be dangerous, especially in women who start with low bone mass prior to menopause. Often, the primary symptom of pathology could be a broken bone, which is called a fracture. The common sites for these fractures ar the hip, spine or wrist.
Diagnosis
Osteoporosis develops gradually, usually without symptoms. A broken bone that happens with minor trauma, such as a slight blow to the wrist, for example, is typically the first symptom. Approximately one in 2 ladies Associate in Nursingd one in four men over age fifty can have an osteoporosis-related fracture in their remaining life.
Both hip and spine fractures are associated with an increased risk of death. Spine fractures, also known as vertebrae compression fractures, occur when weakened vertebrae suffer the impact of a strain, bump or fall. They can result in loss of height, severe and sometimes chronic pain, crowding of internal organs and stooped posture (called kyphosis or “dowager’s hump”). They can also result in prolonged disability and increased mortality.
Hip fractures ar another common consequence of pathology, accounting for one-quarter of osteoporosis-related breaks. A hip fracture will result in a downward spiral of declining health, decreased mobility and increased frailty. They almost always require hospitalization and major surgery and may require long-term nursing home care.
For some, this injury could cause prolonged or permanent incapacity or perhaps death. The number of fractures thanks to pathology is predicted to rise to quite 3 million by 2025, consistent with the National pathology Foundation.
Your health care professional can make a diagnosis of osteoporosis based on your medical history with an assessment of your risk factors; a physical examination and laboratory tests; and a bone mineral density (BMD) test, a noninvasive test that measures your bone mass.
health care professional can make a diagnosis of osteoporosis based on your medical history with an assessment of your risk factors; a physical examination and laboratory tests; and a bone mineral density (BMD) test, a noninvasive test that measures your bone mass.
Common risk factors for osteoporosis are:
- Small, thin frame (weighing less than 127 pounds)
- Personal and/or family history of broken bones or stooped posture in adulthood
- Previous history of osteoporotic fractures of the spine, hip or wrist
- Low lifetime intake of calcium
- Excessive thinness
- Smoking
- Excessive alcohol consumption (“Moderate drinking” for women and older people is defined by the National Institute on Alcohol Abuse and Alcoholism as one drink per day—one drink equals: a 12-ounce bottle of beer (5 percent alcohol) , one 5-ounce glass of wine (12 percent alcohol), or 1.5 ounces of 80-proof distilled spirits. Moderate drinking is considered safe.)
- Inactive lifestyle
- Estrogen deficiency caused by menopause and certain medical conditions such as athletic amenorrhea, anorexia nervosa and treatment with medications that lower estrogen levels
- Absence of menstrual periods or irregular menses as a young woman
- Long-term use of some anticonvulsants and corticosteroids
- Caucasian or Asian ethnic backgrounds, but African-Americans and Hispanic Americans are also at significant risk.
- Certain chronic medical conditions including diabetes, hyperthyroidism, hyperparathyroidism, some bowel diseases and rheumatoid arthritis
- Depression. People with serious depression have increased rates of bone loss, as do people who take selective serotonin reuptake inhibitor (SSRI) antidepressants. More research is necessary to better understand the associations between depression and SSRIs and bone loss.
- Use of proton pump inhibitors. The Food and Drug Administration (FDA) requires safety information on the labels of prescription and over-the-counter labels for proton pump inhibitors about a possible increased risk of fractures to the hip, wrist and spine for people using these medications. Proton pump inhibitors are used to treat a variety of gastrointestinal disorders. They are generally prescribed for a two-week course and are not to be used more than six weeks in a year. In observational studies, the risk rises with prolonged use and high doses of proton pump inhibitors. Further study is needed to verify any increased risk of fractures.
Next Steps
After discussing your individual considerations regarding pathology together with your health care skilled, a series of laboratory tests could also be counseled. These tests can facilitate determine or rule out conditions aside from change of life that will be inflicting low bone density. They include:
- Complete blood cell count
- Blood and urine calcium levels
- Thyroid function tests
- Parathyroid hormone levels
- 25-hydroxyvitamin D test to determine if the body has enough vitamin D
- Biochemical marker tests, such as CTX and NT
If your medical history or physical findings suggest causes of bone loss other than menopause and age, then additional laboratory tests may be conducted.
The U.S. Preventive Services Task Force recommends that girls age sixty five and older be habitually screened for pathology. It additionally recommends screening young women UN agency have a fracture risk adequate to or larger than that of a 65-year-old adult female. In addition, the National Osteoporosis Foundation and the International Society for Clinical Densitometry recommend DXA screening in postmenopausal women and men 50 to 70 who have risk factors for the disease.
It is counseled to possess your BMD performed at a hospital or pathology center that will bone density testing often.
There are several types of BMD tests, including the following:
- DEXA (Dual Energy X-ray Absorptiometry) measures bone density at the spine, hip or total body
- QCT (Quantitative Computed Tomography) could also be wont to live the spine as an alternate to DXA. This test is rarely used, however, because it is expensive and requires a higher dose of radiation. The International Society for Clinical Densitometry (ISCD) recommends DXA as the preferred method for diagnosis or treatment decisions. QCT may be used when DXA is not available, but results are hard to compare with those from DXA.
- Ultrasound uses sound waves to measure bone density. It is most often used in community screening programs to identify individuals who need more definitive testing with DXA bone mineral density testing. The ICSD does not suggest use of ultrasound for designation or treatment selections. Because most of those who have risk for osteoporosis have insurance coverage for DXA testing, paying extra for health screening with ultrasound is rarely necessary.
Results of BMD tests done on postmenopausal women and older men are usually expressed as “T-scores,” a measure of how far your bone density deviates above or below the average bone density worth for a young, healthy, Caucasian lady. For children and young women and men, the better comparison is with individuals of the same age.
- A T-score between +1 and -1 indicates normal bone density.
- A T-score between -1 and -2.5 usually signals low bone density.
- A T-score at or below -2.5 usually signals osteoporosis.
Your bone density is additionally compared to associate “age matched” customary. The age-matched reading (Z-score) compares your bone density to the “norm” for your age, sex and size.
Your T-score can facilitate your health care skilled verify whether or not you’re in danger for a fracture. Generally, the lower your bone density, the upper your risk for fracture. However, your health care skilled can take into account your BMD score in conjunction with your personal health history, pathology risks and style, including whether you exercise and are getting adequate calcium. Your health care skilled may additionally use FRAX, which stands for “Fracture Risk Assessment Tool.” Your FRAX score, which is based on your age, weight, height, medical history and other risk factors, yet as your bone mineral density score, determines your risk of getting a hip or bone fracture within the next ten years. By consideration all of those factors, your health care skilled will verify if pathology poses a big threat for you currently or within the years ahead.
Some tests for pathology risk, such as those available at community health fairs, provide a starting point for assessing your bone health—but definitely require follow-up. If you’ve got one amongst these styles of tests, be sure to discuss the results with your health care professional, especially if your results indicate low bone density.
Medicare and most business insurers get hold of BMD testing for all ladies over the age of sixty-five and for different people in danger or already full of pathology.
Treatment
The primary goal of osteoporosis therapy is to reduce the risk of fractures. A comprehensive pathology treatment program focuses on nutrition, exercise and safety precautions to prevent falls that may result in fractures and, if necessary, medication to slow or stop bone loss, increase bone density and reduce fracture risk. If you’re in danger for or have pathology, your health care professional may recommend several treatment and preventive measures, including:
- Adequate amounts of calcium and vitamin D, either from diet or supplementation
- Regular weight-bearing exercise
- Avoiding smoking and excessive alcohol consumption (“Moderate drinking” for women and older people is defined by the National Institute on Alcohol Abuse and Alcoholism as one drink per day—one drink equals: 12-ounce bottle of beer (5 percent alcohol) , one 5-ounce glass of wine (12 percent alcohol) or 1.5 ounces of 80-proof distilled spirits. Moderate drinking is considered safe).
- Medications to stop or slow bone loss, improve bone density and prevent fractures.
- Surgery to repair broken bones that result from pathology. For example, patients with an acute vertebral fracture and pain that does not respond to standard treatment approaches—medication, increased calcium intake and back-strengthening exercises to improve muscle support—may be candidates for balloon kyphoplasty.Balloon kyphoplasty is similar to a technique known as vertebroplasty, in which acrylic cement is injected into the fractured vertebral bone to stabilize it and relieve pain. During balloon kyphoplasty, however, a small orthopedic balloon is inserted into the vertebrae and inflated with liquid. The balloon is then deflated and removed, creating a cavity into which bone cement may be applied.
- Hip protectors or pads, especially if you are thin or have fallen before.
Medical Approaches to Treating Osteoporosis
The U.S. Food and Drug Administration (FDA) has approved several medications for postmenopausal women to help slow or stop bone loss, build bone and reduce the risk of fractures. These medications work well, but only when they are taken regularly. Plus, as with any medication therapy, there are certain risks and side effects.
- Menopausal Estrogen Therapy and Combination Estrogen-Progestin Therapy Although not approved by the Food and Drug Administration (FDA) for the treatmentof osteoporosis, oral and transdermal forms of estrogen, called estrogen therapy (ET), and combined estrogen-progestin, called hormone therapy (HT), are approved for preventing bone loss in recently menopausal women who have risk factors for osteoporosis, such as low bone mass or a petite frame.Studies notice that ET will increase bone mass and reduces the incidence of bone, radiocarpal joint and hip fractures. However, because of the long-term risks associated with hormone replacement therapy—risks identified within the last several years by the federal Women’s Health Initiative—the FDA recommends that women first consider other pathology medications and warns that internal secretion therapies ought to be used at very cheap attainable dose for the shortest attainable time.
- Raloxifene (Evista)Available in pill kind, this medication is approved for the hindrance and treatment of pathology in biological time ladies. Raloxifene has positive estrogen-like effects on bone however not on the breast or lining of the female internal reproductive organ and will scale back the danger of estrogen-dependent carcinoma by sixty five % over eight years. Raloxifene is currently FDA-approved to decrease the danger of carcinoma in ladies with pathology and even in ladies while not pathology UN agency square measure at high risk of carcinoma.It is part of a class of drugs called selective estrogen receptor modulators (SERMs) that appear to prevent bone loss at the spine, hip and other points in the body. Studies notice that raloxifene reduces the danger of spinal fracture in ladies with pathology, however there are not any information confirming that it reduces the danger of the other fractures. Possible aspect effects embody hot flashes, blood clots within the veins (similar to estrogen) and leg cramps. The pill is taken once a day, with or without meals.
- Alendronate (Fosamax and other brands, including generics) From the bisphosphonate class of drugs, this is a bone-specific medication approved by the FDA to treat and prevent osteoporosis. Studies notice medicinal drug will increase bone mass and reduces the danger of spine, hip, radiocarpal joint and different fractures by up to fifty % over 2 to four years in ladies with pathology.Alendronate has also been approved for the treatment of glucocorticoid-induced osteoporosis and the treatment of osteoporosis in men. Alendronate tablets ought to be taken on associate empty abdomen within the morning and with eight ounces of water a minimum of half-hour before the primary food, beverage or medication of the day. To minimize side effects—which can include heartburn or irritation of the esophagus—remain upright for at least 30 minutes after taking this medication. Alendronate can be taken daily or as a weekly medicine regimen.Alendronate is also available in a pill together with 2,800 or 5,600 IU of vitamin D3, called Fosamax Plus D.
- Risedronate (Actonel, Atelvia)Another form of bisphosphonate drug, this medication is approved to treat and prevent osteoporosis in postmenopausal women and to prevent and treat glucocorticoid-induced osteoporosis in women and men. It may be taken once per day, once per week or once per month. Risendronate is also available with calcium.Studies find risedronate increases bone mass and reduce the risk of spinal, wrist, hip and other non-spinal fractures in women with osteoporosis.Take on an empty abdomen within the morning with eight ounces of water, half-hour before ingestion or drinking. To minimize side effects—which can include heartburn or irritation of the esophagus—remain upright for at least 30 minutes after taking. Take any vitamins, metal and antacids a minimum of half-hour once you’re taking risedronate.
- Ibandronate (Boniva)This is another bisphosphonate that has been approved by the office for hindrance and treatment of pathology in biological time ladies. It reduces the incidence of bone fractures by concerning fifty % and will increase bone mineral density throughout the skeleton. Ibandronate additionally prevents bone loss in recent biological time ladies however UN agency don’t nonetheless have pathology. Ibandronate should be taken once a month on associate empty abdomen, first thing in the morning, with eight ounces of water (no other liquid) at least 60 minutes before eating or drinking. Patients must remain upright for at least one hour after taking this medication. Ibandronate also may be given intravenously once every three months.
- Zoledronic acid (Reclast)A once-yearly infusion of Reclast was approved in 2007 to treat biological time pathology, and a 2009 approval allows it to also be used to prevent onset of osteoporosis in postmenopausal women with low bone mass. Reclast is another bisphosphonate medication that works by strengthening bones and protecting against osteoporosis-related fractures, including those of the spine and hip. In one major study, zoledronic acid reduced risk of hip fractures by 41 percent and spine fractures by 70 percent. Reclast is given just the once a year or once each 2 years (depending on the diagnosis) as a 15-minute endovenous infusion. Side effects embody transient fever, muscle pain, pain in the bones or joints, flu-like symptoms and headache. When these symptoms occur, they usually start within the first three days of receiving Reclast and generally go away within three to four days.
- Calcitonin (Miacalcin, Fortical)This is approved for the treatment of osteoporosis in women who are five years postmenopausal and cannot tolerate estrogen therapy. Studies notice that this medication helps slow bone loss, increases spinal bone density and may relieve fracture pain. Because thyrocalcitonin could be a macromolecule, it cannot be taken orally, so it is taken as a nasal spray or, in some instances, an injection. Possible side effects include nasal irritation and inflammation, bloody nose, headache and backache. Injectable calcitonin may cause an allergic reaction and flushing of the face and hands, frequent urination, nausea and skin rash. Calcitonin is not as potent as different medications for pathology, thus it’s typically reserved for people that cannot take different medicine.
- Teriparatide (Forteo)A form of parathyroid hormone, this is the first medication that stimulates bone formation instead of slowing the breakdown of bone. It is approved for postmenopausal women and for men at high risk for fractures. It increases bone mineral density and reduces spinal fractures and other fractures. The drug is administered by injection once a day (for up to 24 months). Side effects may include nausea, dizziness and leg cramps.
- Denosumab (Prolia)This injectable treatment, approved by the FDA in 2010, is a fully human monoclonal antibody. It offers another option for postmenopausal women with osteoporosis who are at high risk for fracture. It works to decrease the destruction of bone and increase bone mass and strength, and it decreases the risk of spine, hip, and other fractures. An injection is recommended every six months. Side effects may include back pain, pain in the extremities, musculoskeletal pain, high cholesterol levels and urinary bladder infections. Serious adverse reactions include low calcium levels in the blood, serious infections and skin reactions such as dermatitis, rashes and eczema.
There have been some concerns over osteonecrosis of the jaw (ONJ) and atypical fractures of the femur related to osteoporosis medications, particularly bisphosphonates and denosumab. Some reports counsel associate degree multiplied risk of an explicit sort of thigh fracture in individuals with pathology United Nations agency take bisphosphonates for an extended time. As such, the FDA ordered a warning about the link on the Warnings and Precautions section of the labels of all bisphosphonate drugs approved for the prevention and treatment of osteoporosis, and for denosumab.
Sometimes there is some warning pain in the thigh before an atypical fracture occurs, so if you have been taking an osteoporosis medication for several years and start to experience aching or pain in your hip or thigh, contact your health care provider.
Because bisphosphonates accumulate in bone, some patients United Nations agency have taken these medications could also be candidates for a “drug holiday” when five to ten years of bisphosphonate treatment.
It is necessary to acknowledge that ONJ and atypical fractures square measure uncommon, which the chance of a typical hip fracture could be a rather more serious threat to ladies with pathology. Talk to your health care provider about the benefits and risks of taking osteoporosis medication, and discuss what treatment and prevention options are best for you, with your health history in mind.
Preventing Falls Is Key
Preventing Falls Is Key
Falls square measure one amongst the foremost common causes of hip, articulatio radiocarpea and os fracture in individuals over age sixty.
Environmental hazards, like slippery floors or loose floor cover, can increase your risk for falls. Physical issues such as impaired vision and/or balance; chronic diseases that impair mental or physical functioning; and certain medications may also put you at risk.
Consider making some of these changes to help eliminate environmental factors that could lead to falls:
- Indoors: Keep floor surfaces swish however not slippery and away from litter and loose wires; wear validatory, low-heeled shoes even at home; avoid walking in socks, stockings or slippers; be sure stairwells are well lit and that stairs have handrails on both sides; install grab bars on bathroom walls near tub, shower and toilet; and use a rubber mat in the shower or tub.
- Outdoors: If necessary, use a cane or walker for accessorial stability; wear rubber-soled shoes for traction; walk on grass once sidewalks square measure slippery; use caution on extremely polished floors that are slick when wet. Use plastic or carpet runners when possible. Some older ladies at high risk of falls and hip fracture would possibly wish to think about hip protectors. These devices square measure skinny shields that may be incorporated into underclothes.
Prevention
The importance of starting bone loss hindrance at a awfully young age is currently well understood. Bone health programs square measure being developed and enforced that concentrate on women as young as 9 to twelve years older and their oldsters, focusing on promoting good nutritional choices and participating in regular physical activity.
Nearly third of bone loss will occur before a identification of pathology is formed. However, you’ll be able to stop future bone loss caused by pathology with early detection. Also, once you’ve got had a fracture thanks to pathology, your risk of future fractures is multiplied.
Thus, it is important to prevent the first fracture. Taking preventive steps and reviewing risk factors now are especially helpful approaches for women of all ages.
There are five simple steps to reduce your risk for osteoporosis:
- Increase the amount of calcium and vitamin D in your diet.
- Exercise regularly; bones and muscles respond to physical activity by becoming stronger. Weight-bearing exercises like walking and weight lifting are the most beneficial.
- Maintain a healthy body weight. Being underweight or losing weight increases your risk of bone loss and fracture, and ultimately, of developing osteoporosis.
- Quit smoking. Cigarette smoking (nicotine) can reduce bone mass and increase the risk of fracture, thus increasing your risk for osteoporosis. Ask your health care professional to recommend methods to help you quit.
- Drink alcohol in moderation, if you drink. Excessive consumption of alcohol increases your risk of osteoporosis and fractures from falls.
For some women, medication may also be helpful for preventing additional bone loss. Ask your health care professional what the best osteoporosis prevention strategy is for you.
Dietary Strategies for Osteoporosis Prevention
Many vitamins and minerals are important to maintaining healthy bones. That is why it is important to eat a well-balanced diet every day consisting of a variety of foods, including grains, fruits, vegetables, nonfat or low-fat dairy foods or other calcium-rich foods, as well as meat and beans.
Most Americans do not get enough calcium in their diets so adding calcium to your diet may be the easiest health-related change you can make. It’s an important one, too. Calcium could scale back fractures caused by pathology by the maximum amount as fifty p.c. The National pathology Foundation recommends these metallic element tips supported age:
- Girls ages nine to 18: 1,300 mg/calcium/daily
- The average woman age 19 to 50: 1,000 mg/calcium/daily
- Women 51 or older: 1,200 mg/calcium/daily.
If you have asthma, allergies, a thyroid condition or other chronic medical condition, you may need an even higher daily calcium intake. Your intake should not exceed 2,000 mg/day, however.
Good sources of calcium include:
- Low-fat or nonfat dairy products, such as milk, yogurt and cheese. Three eight-ounce glasses of milk plus calcium from a normal diet will meet daily calcium requirements.
- Dark green, leafy vegetables such as broccoli, collard greens, bok choy and spinach
- Sardines and salmon with bones
- Fortified tofu (a soybean product made from curdled soy milk)
- Soy milk
- Almonds
- Calcium-fortified foods and beverages such as orange juice, cereals and breads
Difficulty digesting milk, which is called lactose intolerance, and stomach upset caused by dairy products may be more common as you age. If that’s the case, yogurt with active cultures, buttermilk, and cheddar and Swiss cheeses are high in calcium but low in lactose, the sugar found in milk and milk products.
Many people erroneously believe they’re milk sugar intolerant once an easy sensitivity to farm merchandise or another food substance is de facto the case. So visit your health care skilled before you avoid farm merchandise. Products that do not contain milk sugar (such as Lactaid) will facilitate folks with genetic defect to consume farm merchandise.
When your diet does not offer enough metallic element, you may wish to take calcium supplements. You shouldn’t take calcium supplements you do not need, however. Calcium supplements are available by prescription and over the counter. Always sit down with your health care skilled before you’re taking any new supplement, including calcium.
To choose a metallic element supplement, rummage around for labels that have the u. s. book image or state the supplements area unit pure. Also read the label to determine the amount of elemental calcium (which is the actual amount of calcium in the supplement), Keep in mind that your body best absorbs calcium in doses of five hundred to 600 mg or less, therefore it’s going to be higher to require a number of smaller doses throughout the day (called divided doses). Calcium supplements area unit best absorbed once crazy food.
Multivitamins typically don’t offer enough metallic element to fulfill the daily desires of a biological time lady. In fact, calcium, that could be a mineral, isn’t enclosed in an exceedingly vitamin pill preparation, therefore make certain to scan the label if you’re counting on your nutriment supplement to meet your calcium requirement.
Your diet ought to even be wealthy in calciferol. This nutrient helps your body absorb metallic element additional expeditiously and minimize bone loss. Although the use of dairy products fortified with vitamin D and adequate sun exposure have helped reduce the incidence of vitamin D deficiency, many Americans—particularly older Americans and Americans who live in certain parts of the country—do not get adequate sunlight and are therefore deficient in vitamin D.
This essential vitamin is found in fortified milk and cereals, as well as vitamin supplements. If your exposure to sunlight is limited due to use of sun block or the climate where you live, you may want to consider increasing your average intake of vitamin D. Eight hundred to one,000 units (IU) of calciferol daily is usually recommended for ladies ages fifty, and a few folks could need additional. Check with your health care provider to see how much you need.
Exercise Strategies
Bone and muscle reply to physical activity by changing into stronger. Although all exercise is helpful to overall healthiness, two kinds of exercise are most effective for preventing osteoporosis: Weight-bearing, in which you work against gravity, and resistance exercises, such as weight lifting.
Weight-bearing exercise is any exercise in which your feet and legs bear your weight while you perform it, such as brisk walking, dancing, racket sports and aerobics. This creates high on the bone that helps to make and maintain its strength.
Resistance exercises that strengthen muscle can also be helpful, particularly for the large muscles of the shoulder, pelvis, hips, back and trunk. Because falls area unit the foremost common reason behind fractures, balance-improving activities, such as tai chi and strength training, may also significantly reduce your risk for falls.
In a 2011 British study printed in pathology International, researchers looked at the relationship between regular physical activity and hip fracture risk in middle-aged women. They found women who regularly walked or had moderate or high-frequency physical activities had lower rates of hip fractures compared to women who were sedentary.
The National Osteoporosis Foundation recommends a total of 30 minutes of weight-bearing physical activity on most days of the week, muscle strengthening exercises two to three times per week, and balance, posture and practical exercise a day or as typically pro re nata. Bicycling and swimming are non-weight–bearing exercises and won’t maintain and build new bone, but they are still good for the cardiovascular system.
For muscle strengthening, you can use stationary weight machines at health clubs and gyms and free weights or elastic bands in the gym or at home. The vital factor to recollect is that you just haven’t got to raise significant weights to learn from strength coaching. You should start with a light weight and gradually increase your repetitions and/or resistance as your strength increases. The goal is to make bone strength—not muscle mass, which requires numerous lifts with heavy weights.
In a study World Health Organizationse results shocked even the researchers who conducted it, gardening went a long way to help reduce the risk for osteoporosis among the 3,310 women age 50 and older involved in the study. Gardening activities like raking, thrust a shovel into the bottom and moving a pushcart full of dirt, weeds or mulch area unit all thought-about weight-bearing exercises. Be careful not to lift heavy pots or heavy bags of mulch or dirt.
Facts to Know
- The National Osteoporosis Foundation estimates as many as 54 million Americans have osteoporosis and low bone mass. Research shows about half of women and one-quarter of men will break a bone due to osteoporosis.
- Significant risk of osteoporosis has been reported in people of all ethnic backgrounds.
- Osteoporosis contributes to 2 million fractures annually, including hip fractures, vertebral fractures, wrist fractures and fractures at other sites.
- The number of people beyond age 65 years in the United States is expected to increase dramatically over the next few decades. This will drive up the national cost of osteoporosis, which is estimated at $19 billion per year, according to the National Osteoporosis Foundation. By 2025, the national cost may be as high as $25.3 billion.
- Smoking, abusing alcohol and excessive thinness increase your risk for developing osteoporosis. Likewise, your risk for developing osteoporosis increases if you don’t exercise or if you exercise too much.
- Bones that are calcium rich are less likely to break. Be sure your diet provides at least 1,000 to 1,200 mg of calcium and 400 to 1,000 IU of vitamin D daily, depending on your age, to help keep your bones strong. Drinking or eating three dairy products a day provides the recommended daily intake of calcium, but most women fall short of this requirement. If you are unable to get enough calcium and vitamin D from your diet, your health care professional may recommend a supplement.
- Menopause increases your risk for developing osteoporosis because your body’s natural production of the hormone estrogen declines, and estrogen helps keep bones strong.
- Several types of medications, including raloxifene (Evista), teriparatide (Forteo), denosumab (Prolia), teripartide (Forteo) and bisphosphonates (Actonel, Atelvia, Fosamax, Boniva, Reclast), are effective in preventing and/or treating osteoporosis. Reclast is a single infusion that prevents postmenopausal osteoporosis for two years or treats osteoporosis for a year.
- Women lose the most bone mass—as much as 20 percent—in the first five to seven years after menopause. Because of declining estrogen levels after menopause, a woman’s ability to naturally maintain bone structure is seriously depleted. However, not everyone needs to seek treatment. Bone density testing helps target those at greatest risk for bone loss and osteoporosis.
- A bone mineral density (BMD) test measures the strength of your bones to help assess your future risk of fractures. This test is not usually performed until after menopause, unless you have an unusual clinical situation or are at high risk for osteoporosis. It is quick, painless and noninvasive.
- Bone loss rates can be slowed by regular weight-bearing and muscle-strengthening exercises. Activities such as walking, gardening, jogging and playing tennis help to strengthen bones and connective tissue.
- There is no cure for osteoporosis. However, it is preventable and treatable. You can help prevent bone loss and fractures from osteoporosis with proper diet, exercise and medications, when necessary.
Key Q&A
- Why is osteoporosis called a “silent disease”?Osteoporosis is sometimes called a “silent disease” because it can occur gradually over many years without your knowledge. Often, the very first symptom of osteoporosis is a broken bone, also called a fracture, which typically happens at the hip, spine or wrist. Osteoporosis thins and weakens your bones, making them fragile and more likely to break. However, the good news is that osteoporosis can be prevented and treated. Early detection is important; therefore, you should ask your health care professional for more information about osteoporosis.
- Can’t I just take a multivitamin to prevent osteoporosis?No. Most multivitamins contain only minimal quantities of calcium. Calcium carbonate and calcium citrate are available over-the-counter as supplements if your diet is low in this essential mineral. Girls age nine to 18 need 1,300 mg/calcium/daily. The average woman age 19 to 49 needs 1,000 mg/calcium/daily, and women 50 and older should be getting 1,200 mg/calcium/daily. In addition, be sure your diet (or supplement) also provides between 400 IU (international units) and 1,000 IU of vitamin D (400 to 800 IU for adults under 50 and 800 to 1,000 IU for adults 50 and over), which helps your body absorb calcium. Taking the recommended daily amount of calcium and vitamin D can cut your risk of fracture by as much as 50 percent, particularly in older women. One cup (8 ounces) of fat-free milk contains 306 mg of calcium. Calcium is also found in other dairy products, such as yogurt, cheese and some soy products. Fortified orange and other juices, fortified grains, dark greens and some seafoods are other sources.
- If I’ve already reached menopause, isn’t it too late to do anything about osteoporosis?It’s never too late to make lifestyle changes to improve your bone health and receive the appropriate treatment for osteoporosis, if you have it. Although you can’t restore all the bone that has already been lost, you can build some new bone and prevent bone loss with a diet rich in calcium and vitamin D, a program of weight-bearing exercise and, in some cases, medications.
- Isn’t it true that we get shorter as we age?Substantial loss of height and a stooped posture are not normal results of growing older. Instead, they can be signs of multiple vertebral compression fractures in the spine. Height loss of one- to one-and-one-half inches may be due to degenerative disc disease, however, not necessarily osteoporosis. Frequently, you may not know you have osteoporosis until your bones become so weak that a sudden strain, bump or fall causes a fracture or a vertebra to collapse. It is these collapsed vertebra that lead to loss of height, stooped or rounded posture (called kyphosis, but also known as “dowager’s hump”) and other spinal deformities.
- If I have one or more of the risk factors for osteoporosis, does that mean that I probably have the disease but don’t know it?Not necessarily. Your health care professional will take into account a number of factors in determining your likelihood of developing osteoporosis. These include your personal health history, your individual osteoporosis risks, your lifestyle—including whether you exercise and are getting adequate calcium—and the results of a bone mineral density (BMD) test.
- Is the test for osteoporosis painful?No! A BMD test is safe, quick and painless. Simple measurements are usually taken of the bones in your hip, wrist and spine. You typically remain clothed during the procedure. There are several types of BMD tests; some may use a very small amount of radiation. Talk with your health care professional to learn more about the procedure and to further alleviate any fears you may have about this simple exam and be sure to ask your health care professional what your test results mean when you get them.
- My health care professional recommended that I start working out with weights, but I’m afraid of lifting heavy weights. What should I do?Good news: You don’t have to lift heavy weights to benefit from strength training. You should lift a light amount of weight and gradually increase your threshold as your strength increases. The goal is to build bone and muscle strength—not muscle mass, which requires numerous lifts with heavy weights. So enjoy this important activity and work at your own pace. Just remember, if you do not routinely exercise, ask your health care professional to recommend a simple, safe program and start soon.
- What medications are available to prevent and treat osteoporosis?There are several medications approved by the U.S. Food and Drug Administration for the prevention and/or treatment of osteoporosis. These medications may postpone or stop bone loss, but only when they are taken regularly. Medications currently available include menopausal hormone therapy and the drugs alendronate (Fosamax) adendronate plus vitamin D3 (Fosamax Plus D), raloxifene (Evista), risedronate (Actonel, Atelvia), risedronate with calcium (Actonel with calcium), ibandronate (Boniva), zoledronic acid (Reclast), teriparatide (Forteo), denosumab (Prolia) and calcitonin (Miacalcin). As with any medication therapy, there are risks and side effects associated with each of these medications, but for those with osteoporosis who are have a high risk for fracture, the reduction in fracture risk with treatment can outweigh the risks of treatment. Hormone therapy was once the mainstay of osteoporosis treatment, but it has, for the most part, been replaced with other therapies. Ask your health care professional for more information.



