Facts of Atherosclerosis
Overview
Diseases caused by arterial sclerosis ar the leading explanation for unhealthiness and death for each men and ladies within the us, per the National Heart, Lung, and Blood Institute. Although carcinoma is usually the unhealthiness most feared by ladies, the unwellness affects one out of eight ladies over the period of time, compared to coronary cardiovascular disease, which is responsible for more than one in three female deaths in America. Atherosclerosis is usually the primary stage of coronary cardiovascular disease (CHD).
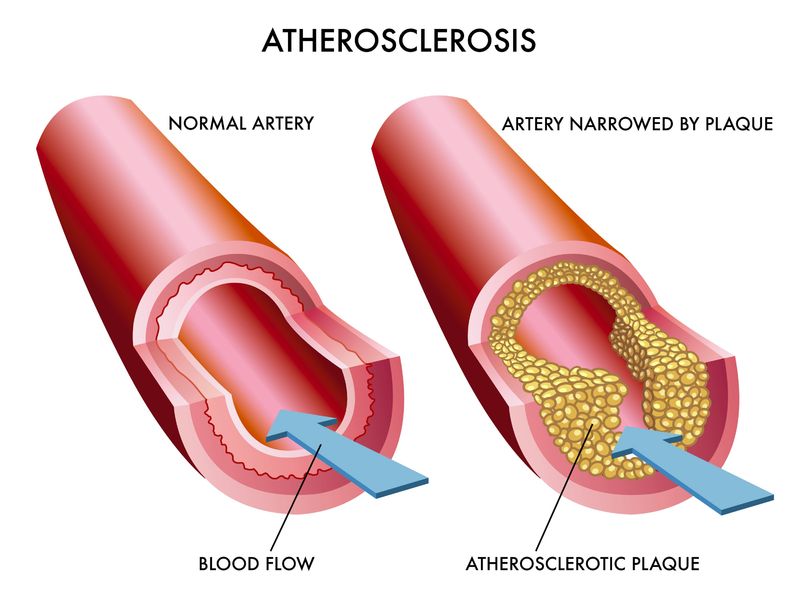
Often noted as “hardening of the arteries,” arterial sclerosis happens once your arteries slender and dwindle versatile. This happens once steroid alcohol, fatty substances, cell waste products, calcium and fibrin—collectively called plaque—collect on the inner walls. The arteries respond to the buildup by becoming inflamed, which, in turn, results in the formation of scar tissue and the collection of other cells in the affected areas, further narrowing the artery.
Atherosclerosis will have an effect on medium and enormous arteries anyplace in your body. If somebody has arterial sclerosis in one a part of their body, they generally can have arterial sclerosis in different components of their bodies. Atherosclerosis restricts blood flow, therefore limiting the quantity of atomic number 8 on the market to your organs. When blood flow to the heart is reduced, for instance, chest pain, or angina, may result. Similarly, once blood flow to the arteries within the legs is reduced, leg pain referred to as gameness might result.
As the unwellness progresses, atherosclerosis can completely clog arteries, cutting off blood flow. This usually happens suddenly when a blood clot forms in the damaged arteries on top of the atherosclerosis. This is particularly dangerous in arteries close to the brain, heart or different very important organs. If blood flow to the center is almost or fully blocked, a heart failure results and muscle cells within the heart die. The result is permanent heart damage. Similarly, if blood flow is abruptly cut off to the brain, this can cause a stroke, which may also result in permanent brain damage. And if blood flow is abruptly cut off to the legs, the leg may have to be amputated. Thus arterial sclerosis will result in serious severe complications if not self-addressed early through hindrance and early treatment.
Atherosclerotic plaques have a cholesterol- or lipid-rich core lined by a fibrous cap. If this cover ruptures, it exposes this lipid-rich core to blood. The sticky core attractsplatelets, forming a grume, referred to as a clot, at the site. This clot will fully clog the artery and discontinue blood flow.
More mature plaques (stable plaques) have a thick fibrous cap, which is less likely to rupture. Softer, fattier plaques (unstable plaques) have a weaker cap and are more likely to rupture.
Surprisingly, the majority of heart attacks occur in arteries that were less than 50 percent blocked before the attack. So the degree of blockage in an exceedingly specific artery doesn’t essentially predict heart failure risk. However, the general total burden of arterial sclerosis throughout all the arteries will have an effect on your risk of a heart failure.
We don’t know what causes plaque to begin building up in arteries. Some experts think plaque begins to accumulate in places where the inner layer of an artery is damaged.
The specific arteries most in danger for atherosclerosis-induced blockage ar those aiming to your brain (carotid), heart (coronary) and legs (femoral or iliac). Atherosclerosis within the legs is that the commonest type of peripheral blood vessel unwellness (PAD) and may result in intermittent claudication—severe pain, aching or cramping when walking, numbness, reduced circulation, and if left untreated, gangrene (death of tissue).
While arterial sclerosis generally progresses gradually—sometimes even beginning in childhood—you ar most in danger once blood vessel blockage builds up quickly, fully separation Associate in Nursing artery. This can happen if the plaque ruptures.
Risk Factors for Atherosclerosis
Over the last two decades, researchers have identified many risk factors for developing cardiovascular diseases. They include:
- Elevated cholesterol levels (both total cholesterol and LDL [“bad”] cholesterol)
- Elevated triglyceride levels
- Low HDL cholesterol (the “good” cholesterol, which clears away artery-clogging LDL cholesterol—the “bad” cholesterol)
- High blood pressure (hypertension)
- Cigarette smoking
- Diabetes (elevated blood sugar)
- Advanced age
High cholesterol. More than half ladies over age fifty five have to be compelled to lower their blood sterol, and 1 / 4 of all yank ladies have blood sterol levels high enough to cause a serious risk for coronary heart disease—a results of arterial sclerosis.
Cholesterol begins aggregation within the walls of the arteries at AN early age. In fact, the earliest style of blood vessel lesion, the “fatty streak,” is present even in young children.
According to the National Cholesterol Education Program (NCEP), elevated LDL cholesterol is a major cause of coronary heart disease. That’s why the NCEP panel recommends aggressive treatment. Treatment might embody fashion changes, such as exercising more and reducing the amount of saturated fat in your diet, and medication. A combination of approaches is typically recommended.
Other lipid abnormalities, such as elevated triglycerides or low HDL (the good cholesterol), are also associated with increased cardiovascular risk.
Cigarette smoking. Smoking accelerates the event of arterial sclerosis, increases blood pressure and restricts the amount of oxygen the blood supplies to the body. Quitting smoking dramatically and now lowers the danger of a attack and reduces the danger of a second attack in those who have already had one.
Diabetes. Having polygenic disease poses as nice a risk for having a attack in ten years as heart condition itself, according to NHLBI. In fact, cardiovascular disease is the leading cause of diabetes-related deaths. People with polygenic disease UN agency haven’t however had a attack have identical risk of future attack as somebody with far-famed coronary heart condition. Because their risk of attack is therefore high, NHLBI recommends that people with diabetes be treated aggressively with LDL cholesterol–lowering medication and carefully manage their blood sugar to reduce their cardiovascular risk.
Age. Generally, ladies over age fifty five and men over age forty five square measure at greatest risk for developing arterial sclerosis. The risk of cardiovascular events increases with age.
Other risk factors for coronary heart disease include:
- A family history of early heart disease (before the age of 60) in a member of your immediate family (parent, sibling, child)
- Obesity
- Metabolic syndrome
- Physical inactivity and sedentary lifestyle
- Postmenopausal status
- Increased levels of high-sensitivity C-reactive protein (CRP), which is a marker ofinflammation
Family History. Even though it’s not enclosed within the Framingham Risk Score, case history is one in all the largest risk factors overall for induration of the arteries. Your risk is greater if your father or brother was diagnosed before age 55, if your mother or sister was diagnosed before age 65 or if you have a sibling with early coronary disease.
Obesity. Overweight girls square measure rather more probably to develop heart-related issues, even if they have no other risk factors. Excess weight in girls is connected with coronary cardiopathy, stroke, congestive heart failure and death from heart-related causes.
Inactivity. Not effort contributes on to heart-related issues and will increase the probability that you will develop alternative risk factors, such as high blood pressure and diabetes.
Metabolic Syndrome. This deadly cluster of risk factors includes five components: abdominal obesity (a large waistline); high blood pressure; glucose intolerance or high fasting blood sugar levels (diabetes or prediabetes); abnormal lipids such as a high triglyceride level; and low HDL (good) cholesterol. If you’ve got 3 out of 5 of those risk factors, you are diagnosed with metabolic syndrome, which is associated with a markedly increased risk of cardiovascular disease.
Stress. though stress has been involved within the development of induration of the arteries, its exact relationship to heart disease has not been determined. Regular exercise will scale back stress and improve your mood.
Postmenopausal status. A woman’s risk of developing induration of the arteries and cardiopathy will increase once she reaches change of life. Prior to change of life, girls square measure principally shielded from cardiopathy by sex hormone, the reproductive hormone produced by the ovaries. This protection is why girls tend to develop cardiopathy ten years when men. However this 10-year protection isn’t seen in girls WHO smoke or have polygenic disease.
Among its many roles, estrogen helps keep arteries free from plaque by improving the ratio of LDL (low-density lipoprotein) and HDL (high-density lipoprotein) cholesterol. It additionally will increase the quantity of HDL cholesterol, that helps clear arteries of lipoprotein cholesterol—the kind that the majority contributes to plaque buildup.
Estrogen additionally helps keep the liner of your blood vessels sturdy and pliable, that helps scale back your risk of induration of the arteries. Despite the theoretical edges of sex hormone, commutation natural sex hormone hormones with medicine when change of life isn’t a good thanks to stop cardiopathy and will even be harmful.
High-sensitivity C-reactive protein. Chronic inflammation has been shown to be a risk factor for cardiovascular disease. While the reasons are not fully known, inflamed atherosclerotic plaques may be more prone to rupture. C-reactive protein (CRP) is a marker of inflammation that can be measured in the blood and is strongly linked to obesity and sedentary lifestyles. However, C-reactive protein has been shown to predict vas risk even on top of ancient risk issue assessment. Weight loss and exercise can lower CRP levels. Statins, a typical category of medicines accustomed treat cholesterin, can also lower CRP. Sometimes doctors will order CRP testing to refine risk prediction among intermediate-risk individuals when the decision to treat with statin therapy is unclear. Older or elderly individuals who have normal or even low levels of cholesterol but who have high levels of CRP may also benefit from statin therapy.
Global Risk Factor Assessment. The Framingham Risk Score may be a helpful, office-based risk prediction model. It assigns some extent score for every major risk issue (age, smoking, total cholesterin, HDL cholesterol, systolic blood pressure) to predict your 10-year risk of developing future CHD events. You can estimate your own 10-year risk at:
If you have more than a 20 percent risk of future cardiac events over the next 10 years, you should be treated very aggressively, the same as someone with known heart disease. Intermediate-risk individuals with scores between 10 percent and 20 percent should have further evaluation. Low-risk people with ample but ten p.c sometimes do not want drug medical care, but should make lifestyle changes such as diet and exercise, which are recommended for everyone.
Recently, many studies have urged that the Framingham Risk Score might underestimate vas risk during a substantial range of people, particularly women and younger adults. The Adult-Treatment Panel (ATP) version of the Framingham Risk Score solely predicts coronary cardiopathy events, but for women under the age of 75, strokes are more common than the CHD events predicted by the risk calculator. Certain people with low- or intermediate-risk Framingham Risk Scores could also be candidates for alternative testing if they need alternative risk factors like a powerful case history that square measure not included in the Framingham Risk Score.
Women and young adults usually have low Framingham Risk Scores for short-run risk over consecutive 10-years however have substantial period of time risk. Even the presence of 1 major vas risk issue by the age of fifty is related to hyperbolic period of time risk of upset and shorter median survival compared to women with optimal risk factor status. Thus “low-risk” over consecutive ten years isn’t an equivalent as “no risk,” and it is imperative that risk factors are screened for and treated appropriately. It is necessary to stop risk factors from developing through a healthy life style.
Recently, another global risk assessment tool called the Reynolds Risk Score was developed, which has been shown to have improved predictive ability for all cardiovascular events compared to the Framingham Risk Score. This tool incorporates several of the standard risk factors employed in the Framingham Risk Score, however adds 2 alternative necessary risk factors: case history of premature arteria coronaria sickness and high-sensitivity C-reactive protein. You can estimate your 10-year risk
Both risk assessment tools were developed among predominantly Caucasian populations and may not apply well to individuals from other races or ethnicities.
Symptoms of Atherosclerosis:
Often, you’ll expertise no symptoms of malady|arteriosclerosis|arterial sclerosis|hardening of the arteries|induration of the arteries|coronary-artery disease} till the disease has progressed considerably. However, there ar some conditions that will counsel coronary-artery disease is gift, though these conditions could happen for alternative reasons.
- Angina.If clogged arteries prevent enough oxygen-carrying blood from reaching your heart, the heart may respond with pain called angina pectoris. Episodes of angina occur once the center’s would like for O will increase on the far side the O out there from the blood nutrient the heart. Silent angina happens once an equivalent inadequate blood provide causes no symptoms.Physical exertion is that the commonest trigger for angina. Other triggers is emotional stress, extreme cold or heat, heavy meals, alcohol and cigarette smoking. The pain is a pressing or squeezing pain, usually felt in the chest or sometimes in the shoulders, arms, neck, jaws or back.Angina suggests that coronary heart disease exists. People with angina have an increased risk of heart attack compared with those who have no symptoms. When the pattern of angina changes—if episodes become a lot of frequent, last longer or occur while not exercise—your risk of attack in later days or weeks is far higher and you should see your health care professional immediately.If you have angina, learn its pattern—what causes an angina attack, what it feels like, how long episodes usually last and whether medication relieves the attack. Angina is usually relieved in a few minutes by resting or taking prescribed angina medicine, such as nitroglycerin.Episodes of stable angina seldom cause permanent damage to heart muscle.Heart attack pain is also like angina, however the symptoms of angina quickly disappear with rest. Heart attack pain, however, usually persists despite resting or taking nitroglycerin and should be evaluated immediately. Like angina, heart attack pain can be a pressure or tightness in chest, arms, back or neck.Often symptoms include shortness of breath, sweating, nausea, vomiting, indigestion or dizziness.
Women, particularly those with polygenic disorder, may not have the typical symptoms of chest pain like men, but have other symptoms such as shortness of breath or indigestion. A heart attack is an emergency. A delay in treatment might mean a lot of of the center muscle tissue is for good broken.
If you think that you’re having a attack, call 9-1-1. After you call 9-1-1, the operator may recommend that you chew one adult-strength (325 mg) aspirin after he or she makes sure you don’t have an allergy to aspirin or a condition that may make taking it too risky. If the operator does not seek advice from you concerning manduction associate salicylate, the emergency medical technicians or physicians at the hospital can provide you with one if it’s right for you. - Cardiac arrhythmias. These occur once the center momentarily beats too quick or beats on an irregular basis. Chest pain, dizziness and shortness of breath are symptoms of cardiac arrhythmias. Atherosclerosis is one explanation for speedy or irregular heartbeat; but, it can also be caused by angina, valvular heart disease, blood clots,thyroid abnormalities, electrolyte imbalance or previous heart damage. Arrhythmias may be frequent or infrequent.
- Silent ischemia. Sometimes atherosclerosis causes no symptoms. Silent ischaemia could be a condition caused by coronary-artery disease, but isn’t associated with the chest pain or other symptoms common to other types of heart conditions. This condition happens once arteries with coronary-artery disease cannot deliver enough blood to the center. An electrocardiogram (EKG or ECG), a measurement of electrical impulses produced by the heart, may indicate silent ischemia. However, unless you recognize your risks for heart condition and choose, with the advice of your health care professional, that you need a heart checkup, you may never know you have ischemia. People with polygenic disorder ar particularly in danger for this condition.
- Intermittent claudication. This leg disorder predominantly affects elderly people. It causes severe pain, aching or cramping in the legs when you walk due to atherosclerosis in the major arteries that supply blood to the legs (femoral and iliac). Severe cases of peripheral arterial disease can lead to gangrene andamputation.
- Transient ischemic attack (TIA) and strokes. If you experience a sudden onset of weakness or numbness on one side of your face, arm or leg, or an inability to talk or find words, or lose vision in one eye, you may be having a stroke or a TIA.Neurological symptoms that last less than 24 hours are called TIAs, whereas symptoms that persist for longer are classified as strokes.TIAs and strokes are often the result of atherosclerosis in the arteries that supply blood to the brain, such as the carotid arteries. This is very serious. If you think that you’re experiencing a stroke, you should call 9-1-1 to seek medical attention immediately. This is the brain’s equivalent of a “heart attack,” during which the brain is deprived of oxygen-carrying blood supply. Any delay in medical treatment could for good harm your brain.
Diagnosis
The earlier atherosclerosis is diagnosed the better. You’ll want to take many of the following steps to determine if you’re at risk for this condition. Discuss different steps listed below along with your health care skilled.
- Office-based Physical Exam. All ladies ought to bear associate annual examination to assess their risk factors for upset and for any symptoms of induration of the arteries. The physical exam should include measuring your blood pressure and height and weight to calculate a body mass index (BMI). A normal blood pressure is less than 120/80. If you have high blood pressure, you should see your health care professional more frequently to make sure your blood pressure is being adequately treated to the goal of less than 130/85. If you’re overweight, you have a higher risk of diabetes and metabolic syndrome. Your doctor ought to encourage you to follow a healthy diet and to exercise frequently to scale back your risk.Often, atherosclerosis is not diagnosed until you have complications. However, before you expertise complications, your health care professional may be able to hear a blowing sound called a bruit when holding a stethoscope over a damaged artery. Also, you may have a decreased pulse in the affected area. Sometimes, induration of the arteries causes the pressure in every of your arms to be considerably totally different, another symptom your health care professional can easily check. More usually, there are no apparent signs on physical exam to suggest the presence of atherosclerosis, and thus individuals with risk factors may be referred for additional testing.
Laboratory tests. Beginning at age twenty, women should have their blood cholesterol measured. If it is normal, it can be rechecked every five years. However, if it is abnormal, it should be monitored more frequently, such as at least once a year. A complete conjugated protein level (a biopsy that measures total cholesterin, LDL cholesterol, HDL cholesterol and triglyceride levels) is recommended by NHLBI as the initial test to determine if your cholesterol levels are within normal ranges. This type of test, called a fasting lipoprotein test, is taken when you haven’t eaten for a prescribed amount of time—usually between nine and 12 hours. Blood-level cholesterol is measured in milligrams per deciliter (mg/dL; a deciliter is one-tenth of a liter).If you are at risk for high cholesterol or other conditions that contribute to the development of cardiopathy, your health care professional may recommend more frequent testing.Here are “at-a-glance” guidelines for your cholesterol levels. Be sure to raise your health care skilled if your blood cholesterin goals ought to diverge supported anyone cardiopathy risks you will have, like polygenic disorder and high blood pressure, or if you smoke:
- Total cholesterol levels:
Desirable: less than 200 mg/dL
Borderline high-risk: 200 to 239 mg/dL
High risk: 240 and above - HDL (high density lipoprotein) levels:
Optimal: above 60 mg/dL. (considered protective against heart disease.)
40 to 50 mg/dL: the high the level the less your risk for heart disease
Less than 40 mg/dL: considered a major risk factor for heart disease - LDL (low-density lipoprotein) levels:
Optional goal for high-risk patients: less than 70 mg/dL
Optimal: less than 100 mg/dL
Near optimal:100 to 129 mg/dL
Borderline high: 130 to 159 mg/dL
High: 160 to 189 mg/dL
Very high: 190 mg/dL and above
According to NHLBI’s updated 2004 cholesterol guidelines:
For individuals at terribly high risk for coronary failure, like people who have had a recent coronary failure or unstable angina, the general cholesterin goals ought to be less than seventy mg/dL; drug medical aid with statins is typically counseled to succeed in this goal.
For patients at high risk for coronary failure, cholesterin goals ought to be but a hundred mg/dL with associate ex gratia goal of but seventy mg/dL, and drug medical aid is usually recommended to reach these goals. High-risk individuals include people with known atherosclerosis (such as those with a prior heart attack, stroke or peripheral arterial disease), people with diabetes or kidney disease or people with enough risk factors to give them a 10-year risk of a heart attack of more than 20 percent under the Framingham Risk Score. Studies suggest that high-risk and very high-risk patients may benefit from statin therapy even if their cholesterol levels are not elevated to prevent further events.
For moderately high-risk patients: LDL cholesterol goals should be set for less than 130 mg/dL (or better yet, less than 100 mg/dL) and drug therapy should be used at LDL levels of a hundred to 129 mg/dL to succeed in this goal. Moderately insecure people embody those whose ten-year risk of a coronary failure is 10 % to twenty %, those with over 2 risk factors for heart condition, those with a positive case history of premature coronary illness or those with the metabolic syndrome.
For low-risk patients, cholesterin goals ought to be but a hundred and sixty mg/dL. Low-risk people area unit those whose ten-year risk of heart condition is a smaller amount than 10 %, and who have less than two risk factors for heart disease. Usually, lifestyle changes such as diet and exercise are recommended first, but drug therapy can be added if these are not enough to meet their goal.
Note that way changes like diet and exercise area unit counseled for everyone—even those on drug therapy! When lifestyle changes alone are not adequate, the most common class of medications used to treat high cholesterol is called statins (examples include atorvastatin (Lipitor), simvastatin (Zocor), rosuvastatin (Crestor), pravastatin (Pravachol), lovastatin and fluvastatin). Statins are highly effective in reducing cholesterol levels and also reduce the risk of having a first or recurrent heart attack.
In fact, while there are several types of cholesterol-lowering medications available, at this time the group of cholesterol medications called statins have been shown to be the most effective at reducing cardiovascular events. Thus, if cholesterol-lowering medications area unit indicated, statin therapy should be the first therapy used for preventing subsequent cardiovascular events in most individuals, especially in high-risk and very high-risk individuals. If an individual cannot tolerate one particular statin due to side effects, usually other types of statins at lower doses can be tried. Once a personal is maximized on the best dose of lipid-lowering medicine tolerated, if their cholesterin continues to be not at goal, another class of sterol medications are often side to their regimen.
- Triglyceride (another type of lipid) levels:
Ideal: Less than 100 mg/dL
Normal: less than 150 mg/dL
Borderline high: 150 to 199 mg/dL
High: 200 to 499 mg/dL
Very high: 500 mg/dL and higher
Normal triglycerides are considered less than 150 mg/dL. If you’re at moderate or high risk for heart disease and still have high triglycerides (despite reaching your cholesterol goal with a statin), you may require an additional medication. This includes a fibrate like medication (Lopid) or B-complex vitamin. Fish oil and polyunsaturated fatty acid fatty acids can also facilitate scale back lipid levels.The main target of medical aid is achieving your low-density lipoprotein goal. A secondary target is your non-HDL cholesterol. Non-HDL is your total cholesterol minus your HDL cholesterol. This number reflects some of the other atherogenic lipid problems, such as elevated triglycerides. The non-HDL goal is usually thirty points on top of your low-density lipoprotein goal. For example, if your low-density lipoprotein goal is a smaller amount than one hundred mg/dL, your non-HDL goal is less than 130 mg/dL). Specific treatment depends on your cholesterol level and other risk factors, but in general, the first stage of treatment is lifestyle changes, such as improvements in diet and exercise. If lifestyle changes don’t work, statin drugs are usually tried first, and other medications may be added if necessary. - LDL particles. Cholesterol is carried into the vessel wall through particles known as lipoproteins. Depending on its size, every particle carries totally different amounts of sterol among it. Many patients with polygenic disorder or metabolic syndrome don’t have elevated blood levels of total or LDL cholesterol, however they need elevated triglycerides and low levels of the great HDL cholesterol. This is related to a pattern of little, dense LDL-particle size, which is linked to promoting atherosclerosis.A standard lipid blood test will give you the LDL level concentration but does not tell you concerning your total particle count. In sure cases once additional data is required to work out your risk, your doctor may order tests to measure your LDL particle size or your total LDL particle count. In a given supermolecule blood concentration, there will be more total particles if your particle size is small and fewer total particles if your particle size is large. There is conjointly a take a look at known as apolipoprotein B (apoB), which is a good estimate of your total count of the bad atherogenic particles.
Your doctor could order blood tests apart from supermolecule levels, to work out your risk of cardiovascular disease. These include:
- Fasting sugar (high levels may mean diabetes or prediabetes)
- Insulin levels (high levels may mean diabetes or prediabetes)
- Kidney function (abnormal kidney function is a risk factor for heart disease)
- C-reactive protein (high levels of CRP suggest inflammation in the body and is a marker for increased risk of heart disease)
- Ankle brachial index. This simple check performed in a very health care professional’s workplace screens for peripheral blood vessel sickness (PAD). The pressure reading measured in every leg is split by the typical pressure reading in each arms. Normally, the pressure within the legs is that the same or over the pressure within the arms, so a value of 1 or higher is normal. An ABI of less than 0.90 suggests peripheral arterial disease. Even if you don’t have any symptoms, but do have PAD, you should be treated aggressively with medical therapy because you have a higher risk for future cardiovascular events, including heart attacks and strokes.There are other tests that can help your health care professional determine if you have atherosclerosis. These are:
- Coronary angiography (or arteriography). This test is used to explore the coronary arteries. A dye is injected into the artery of associate degree arm or leg via a fine tube, or catheter that passes through the aorta into the arteries of your heart. Your heart and blood vessels are then filmed while your heart pumps. The picture that’s seen, called an angiogram or arteriogram, shows any blockages caused by atherosclerosis, as well as other problems. This is an invasive test and is only used for high-risk individuals who are believed to have a good chance of having significant coronary heart disease.This is the most accurate way to assess the presence and severity of coronary disease. Sometimes this is done in combination with an ultrasound probe, which is passed through the catheter down into the coronary arteries. This procedure is called intravascular ultrasound or IVUS. IVUS permits for even higher detail of the blood vessel wall to assess the severity of a lesion and therefore the sort of plaque buildup, such as “soft” plaques vs. “hard” plaques.You may even be injected with a fluid that blocks X-rays, called a “contrast medium” or “dye,” which allows getter visibility of certain tissues. The injection might sting and leave a argentiferous style in your mouth, a warm or cool sensation at the injection site and in some cases, hives. Many of these dyes are iodine-based, so you need to tell your health care professional if you are allergic to iodine.If your health care professional decides that you need to have associate degree roentgenography, you may have to fast four to six hours before the test because of the sedative medications you receive during the test.If a significant blockage is found during the angiogram, the cardiologist may try to open up the blockage with a balloon with or without a stent—a process called angioplasty.
- Imaging tests. To study your arteries to determine whether or not you have hardening or narrowing of large arteries or calcium deposits on artery walls or to determine other information about the structure or function of your heart, your doctor may use imaging techniques such as a computerized tomography (CT) scan or a magnetic resonance angiogram (MRA), a noninvasive test that gives similar information to a CT scan without using X-rays.A non-contrast cardiac CT can detect calcium buildup in the arteries, which is a marker of atherosclerotic plaque (calcium shows up on the CT as bright white, similar to bone, and can be seen without contrast). This is called a coronary artery calcium (CAC) score and is sometimes ordered in intermediate-risk individuals for screening when further assessment of CHD risk is needed. People with high levels of CAC have a lot of plaque in their arteries, which is associated with increased risk of cardiovascular events. If you have high CAC scores, more intensified treatment such as statins may be recommended, in addition to lifestyle changes.A cardiac CT with dye contrast (called a CT angiogram or CTA) can further show whether there is any narrowing or stenosis of the coronary arteries. Because CTAs have the increased risk of dye and increased radiation compared to non-contrast CTs, they are not recommended for routine screening where no symptoms are present but may be used for evaluation if you have chest pain or angina.
- Doppler ultrasound. Your doctor might use associate degree ultrasound tool known as a Doppler ultrasound to require your pressure at totally different points on your arm or leg. By measurement these pressures, your doctor can gauge the blood flow through your arteries as well as the degree of any blockages.
- Resting EKG. An graph might show signs of previous heart injury like associate degree megalocardia or areas of previous coronary failure. For many women with angina, the EKG at rest is normal. This is not shocking as a result of symptoms of angina occur throughout stress. Therefore, your heart’s functioning could also be tested beneath stress, typically exercise.
- Exercise stress test. This check shows however well the guts functions with inflated physical activity. An graphical record and pressurea} are taken before, throughout and when the effort. Other stress tests in addition to the EKG use radionucleotide markers such as thallium, or ultrasound (echocardiography), to take pictures of the heart before and after the stress to look for changes in the heart that might suggest blockages. Usually the stress test involves running on a treadmill, but if you can’t use the treadmill, the heart can be stressed using medications such as dobutamine or adenosine or some newer stress agents similar to adenosine.
Treatment
Lifestyle changes (Diet, exercise, weight loss):
- Diet. Changing your dietary habits remains the one best thanks to stop induration of the arteries from progressing. Eating a diet low in saturated fat and steroid alcohol reduces blood steroid alcohol, a primary reason behind induration of the arteries. Although saturated fat and trans fats are definitely bad for you, other types of fat, such as polyunsaturated fats found in fish (omega-3), nuts and flaxseed, or monounsaturated fats found in olive oil, may be good for you. Eating less saturated fat and reducing calories in general should also help you lose weight.In addition to watching saturated and trans fats, it is also important to watch excess sugar intake, like sugar, honey and high fructose corn syrup, which are frequently found in sweetened beverages and desserts and also hidden in many processed foods. The body can convert excess calories like from sugars into triglycerides as the way of storing energy. So lowering your sugar intake will also lower your triglyceride levels, in addition to your blood glucose levels.Reducing sodium intake is important for both the prevention and treatment of high blood pressure. The DASH (Dietary Approaches to Stop Hypertension) diet, endorsed by the major heart organizations, is one strategy for lowering high blood pressure. It is rich in lower-calorie foods such as fruits and vegetables and whole grains and low in sodium.The Therapeutic Lifestyle Changes (TLC) Diet plan, developed by the NHLBI calls for less than seven % of your calories to come back from saturated fat and for fewer than two hundred mg of dietary steroid alcohol. Twenty-five percent to 35 percent or fewer of total daily calories can come from fat, provided most of these calories are from unsaturated fat, which doesn’t raise cholesterol. Sodium intake should be limited to no more than 2,400 mg per day. In addition, the guidelines encourage the use of certain foods rich in soluble fiber to boost the diet’s LDL-lowering power.
- Exercise. You also can benefit from exercise. Recent analysis finds that even moderate amounts of physical activity area unit related to lower death rates from coronary cardiopathy. As very little as half-hour of moderate activity on most, and preferably all, days of the week helps protect the heart and is recommended by the American Heart Association. However, the recommendations rise to sixty to ninety minutes of moderate activity most, and preferably all, days of the week in women who need to lose or maintain weight. Examples of moderate activity area unit brisk walking, bicycling, raking leaves and gardening. Vigorous exercise includes running, jogging, swimming laps and cross-country skiing. Being physically work and active provides vessel advantages freelance of weight loss.Wearing a pedometer may help you keep track of your physical activity. The American Heart Association recommends aiming for 10,000 steps a day, which is five miles (2,000 steps per mile), but all steps count. Aim to get more steps in your day by taking stairs instead of elevators, parking farther away and other small changes.
- Weight loss. If you’re overweight, losing weight can help lower blood cholesterol levels. It is additionally the foremost effective fashion amendment to scale back high force per unit area, another risk factor for atherosclerosis and heart disease. The best thanks to change state is thru a mix of diet and exercise.
Pharmacologic (drug) therapies:
- Anti-platelet (or blood-thinning) medications. Your doctor may prescribe an anti-platelet medication, such as aspirin or clopidogrel (Plavix) to reduce your chances of a blood clot if you have atherosclerosis or are at high risk for it.
- Anticoagulants. Anticoagulants, such as heparin or warfarin (Coumadin), can also help prevent clots from forming. Warfarin may be prescribed if you have heart arrhythmias called atrial fibrillation or flutter or if you have had certain types of strokes. Newer anticoagulants, such as dabigatran, rivaroxaban and apixaban, can be used in place of warfarin for certain indications like atrial fibrillation.
- Cholesterol-lowering therapies. Cholesterol- and triglyceride-lowering medications which will be suggested include:
- Statins. Six statin drugs are available in the United States: atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Mevacor, Altoprev), pravastatin (Pravachol), simvastatin (Zocor) and rosuvastatin (Crestor). In addition, statins are found in the combination medications lovastatin and niacin (Advicor), atorvastatin and amlodipine (Caduet), and simvastatin and ezetimibe (Vytorin). Statins are most effective at lowering the LDL cholesterol, but they may also have modest effects on raising HDL cholesterol and lowering triglycerides. They are generally the first-line medications used.Make sure you talk to your health care professional to see if you are a candidate for statin therapy. If you expertise any facet effects like muscle aches or dark excreta, stop taking the drug immediately and call your health care professional.
- Niacin. Niacin is a water-soluble B vitamin. Unfortunately, you can’t lower your cholesterol by taking a vitamin supplement; to have such an effect, it must be taken in doses well above the daily vitamin requirement. Although B is cheap and out there over the counter, never take it to lower your cholesterol without guidance from a health care professional because of potential side effects. The extended unleash type is obtainable by prescription as Niaspan. It decreases triglycerides, raises HDL-cholesterol and modestly lowers LDL-cholesterol. Unfortunately, this medication causes some people to itch and flush (turn red).
- Bile acid sequestrants. The three main bile acid sequestrants currently prescribed in the United States are cholestyramine resin (Questran), colestipol (Colestid) and colesevalam (WelChol). Available as powders, tablets or granules, these drugs work by binding with bile acids that contain cholesterol in the intestines. They can be prescribed alone or in combination with another drug.
- Fibrates. These medication cut back triglycerides by reducing the liver’s production of cholesterol and aiding within the removal of triglycerides from the blood. The most wide used fibrates within the us ar medicinal drug (Lopid) and fenofibrate (Tricor). Fibrates aren’t suggested because the sole drug medical care for girls with cardiopathy for whom cholesterol reduction is that the main goal.
- Cholesterol absorption inhibitors. This class of drugs lowers cholesterol by preventing it from being absorbed in the intestine. The first approved drug in this class is ezetimibe (Zetia). It may be used alone or together with a statin.
- Omega-3 fatty acids. Omega-3 fatty acids like animal oil could also be facilitate raise cholesterin and lower elevated triglycerides. It can be given in a prescription form or over the counter.
Drugs for peripheral arterial disease
If you have got severe pain or cramping in your legs after you walk, your health care skilled might advocate clopidogrel (Plavix), cilostazol (Pletal) or Trental (Trental). Cilostazol is generally avoided in individuals with congestive heart failure.
If you are taking medication to boost your cholesterin, lower blood pressure or treat other heart disease symptoms, be sure to ask about potential side effects; interactions with other medications, food or beverages; and when and how you should take the prescribed medications.
Revascularization procedures for atherosclerosis
In the past, opening arteries damaged by atherosclerosis around the heart meant performing bypass surgery (open heart surgery), requiring that the chest be opened surgically and blood flow redirected around the damaged artery. Now, alternatives to open surgery, such as balloon angioplasty, allow for a quicker, less painful recovery. However, not everyone is a candidate for balloon angioplasty and some people still require surgery. Also, not everybody with induration of the arteries needs gap the arteries with surgical operation. Some people with stable arteria sickness and stable angina is also candidates for treatment with aggressive medical medical aid alone. These selections depend upon the individual, the types of blockages, the results of stress testing, the severity of symptoms and other factors.
- Coronary angioplasty or balloon angioplasty. Your health care skilled can 1st perform a coronary X-ray picture to examine that arteries ar blocked. Through a tubing (or tube) in your leg (femoral) or arm (brachial) artery, a tubing are advanced to the center and dye are injected into the coronary arteries. If surgical operation is indicated, the heart surgeon can position a tubing with a small balloon on its basketball shot the narrowed coronary. The balloon is inflated and deflated to stretch or break open the narrowing and improve the passage for blood flow. Typically, your doctor will insert a stent, a small scaffolding designed to prop the artery open. As the balloon inflates, it expands the stent. Angioplasty is not surgery, and it is performed while you are awake. It typically takes about one or two hours. But there’s recovery time that usually involves birth flat for 3 to 6 hours once the procedure to permit the leg (or arm) artery to heal to stop bleeding.If angioplasty doesn’t widen the artery or if complications occur, bypass surgery may be needed. Patients with bound kinds of blockages might not be candidates for surgical operation and should be referred for bypass surgery.One continuing challenge cardiologists face in treating atherosclerosis is that plaque deposits may return (a condition referred to as restenosis). Even patients who’ve had angioplasties sometime require future treatments to widen arteries clogged with new blockage. Today, new drug-coated stents markedly decrease the rates of restenosis compared to the older generation of stents. Additionally, new drugs and new types of stents are in development, and the future is promising for advancements in this area.
- Atherectomy. Coronary atherectomy is a procedure that removes plaque from the arteries that supply the heart muscle using a rotating shaver or laser catheter. Atherectomy is also followed with stenting or balloon surgical operation.
- Endarterectomy. This surgical procedure, performed under general anesthesia, removes plaque from your arteries. For your carotid arteries, the surgeon makes a cut in your neck, opens the artery there, and removes plaque until the inside of the artery is clean and smooth.
- Thrombolytic therapy. If a blood clot is blocking an artery, your doctor may insert a drug directly into that artery at the point of blockage to break up the clot at the time of angiography. During an acute heart attack, if angioplasty is not immediately available at your hospital, doctors may give thrombolytic therapy vein to break up clots in your body. There ar some risks to therapy as well as injury within the brain. Thus if angioplasty is available, this is generally preferred to systemic thrombolytic therapy for heart attacks.
- Coronary artery bypass. In this surgery, a blood vessel (usually taken from the leg, arm or chest) is sewn onto the blocked artery so blood can bypass the blocked area. Several bypasses can be performed if several arteries are blocked. Bypass surgery relieves symptoms of cardiovascular disease however doesn’t cure it. You will still need to make lifestyle changes like those described earlier and take medications.
Prevention
Try to follow these tips to prevent atherosclerosis:
- Quit smoking. Smoking accelerates the event of hardening of the arteries, which frequently ends up in coronary heart condition. Women WHO smoke square measure 2 to 6 times as doubtless to suffer a heart failure as nonsmoking ladies, and therefore the risk will increase with the amount of cigarettes smoke-dried per day. The good news is that quitting dramatically cuts your risk, even during the first year, no matter what your age.
- Lower your blood pressure. Even slightly high pressure level levels will double your risk for heart condition. Normal pressure level is a smaller amount than 120/80 millimeter of mercury. High blood pressure, or hypertension, is a blood pressure reading of 140/90 mm Hg or higher. Between 120/80 mm/Hg and 139/89 mmHg is taken into account prehypertension.High pressure level conjointly will increase your likelihood of stroke, symptom heart disease and renal disorder. High blood pressure can be treated successfully with medication. Commonly prescribed drugs include diuretics, angiotensin-converting enzyme inhibitors (ACE inhibitors), angiotensin II receptor blockers, beta blockers and calcium channel blockers (CCBs).If your blood pressure is not too high, you may be able to control it entirely through weight loss (if you are overweight), regular physical activity and cutting down on alcohol, as well as salt and sodium. Sodium is an ingredient in salt that is found in many packaged foods, carbonated beverages, baking soda and some antacids.
- Get regular exercise and lose weight. Fortunately, it doesn’t take a lot of time or effort to become physically active. As very little as half-hour of moderate activity on most, and ideally all, days of the week helps defend the center and is suggested by the yankee Heart Association. The recommendations rise to sixty to ninety minutes of moderate activity most, and preferably all, days of the week in women who need to lose or maintain weight. Examples of moderate activity square measure brisk walking, bicycling, raking leaves and gardening. Vigorous exercise includes running, jogging, swimming laps and cross-country skiing.You can divide the 30 to 90 minutes of moderate activity into shorter periods of at least 10 minutes each. If you already engage in this level of activity, you can get added benefits by doing more.
- Control your blood sugar if you have diabetes. Diabetes is often diagnosed by a fast aldohexose (sugar) over one hundred twenty five mg/dL. Patients with polygenic disease ought to be treated to forestall complications from vessel disease; treatment usually consists of a mix of modus vivendi changes and medications. Your goal hemoglobin A1C with treatment should be less than 7 percent. Those with diabetes who also have good sugar control are much less likely to develop cardiovascular complications than those with poor sugar control.Those individuals with a fasting glucose (sugar) of a hundred to one hundred twenty five mg/dL is also thought of prediabetes or aldohexose intolerant. This is typically related to metabolic syndrome, and individuals with glucose intolerance are at high risk for developing true diabetes within the next 10 years. Weight loss, healthy diet and exercise are important to improve blood sugar levels and prevent the onset of diabetes.
- Lower your LDL-cholesterol level. According to the Centers for illness management and hindrance, about one in every six adults—or 16.3 percent of the United States adult population—has high total cholesterol. More women have high cholesterol than men.
- Keep triglycerides in check. The conjugated protein profile that determines your cholesterin levels conjointly measures another fatty substance referred to as lipide. Produced in the liver, triglycerides are made up of saturated, polyunsaturated and monounsaturated fats. The optimal target triglyceride level for individuals without heart disease or heart disease-related risk factors is less than 100 mg/dL.For most people, cutting back on foods high in saturated fat and cholesterin and intake a lot of fiber can lower each total and cholesterol. Regular physical activity and weight loss if you are overweight conjointly reduces blood cholesterin levels. Losing additional weight, quitting smoking and becoming more physically active may also help boost HDL cholesterol levels. Losing weight, effort and restricting on sugar intake will facilitate lower triglycerides.
Facts to Know
- Atherosclerosis is often the first stage of coronary heart disease.
- Diseases caused by atherosclerosis are the leading cause of illness and death in the United States.
- Atherosclerosis occurs when your arteries narrow and become less flexible because cholesterol, fatty substances, cell waste products, calcium and fibrin—collectively called plaque—collect on their inner walls. The arteries respond to the buildup by becoming inflamed, causing scar tissue and other cells to form in the affected areas, further narrowing the artery.
- What causes plaque to begin building up isn’t known. Some experts think plaque begins to accumulate in places where the inner layer of an artery becomes damaged, possibly by elevated cholesterol levels, elevated triglyceride levels, high blood pressure or cigarette smoke.
- A woman’s risk of developing atherosclerosis and heart disease increases as she ages. Prior to menopause, estrogen produced in the ovaries provides some protection from heart disease. However, hormone replacement in women after menopause does not reduce the risk of cardiovascular disease. And remember that women with diabetes or those who smoke are at risk for heart disease throughout their lives.
- Atherosclerosis can affect medium and large arteries anywhere in your body, restricting blood flow and limiting the amount of oxygen available to organs.
- Smoking accelerates the event of induration of the arteries, will increase pressure level and restricts the quantity of gas the blood provides to the body.
- Changing modus vivendi habits remains the only handiest thanks to stop the induration of the arteries from progressing. Changing your diet to at least one low in fat, particularly saturated fat, and steroid alcohol helps scale back high blood steroid alcohol, a primary cause of atherosclerosis.
- If you are overweight, losing weight will facilitate lower blood steroid alcohol. It is the foremost effective modus vivendi modification for reducing high pressure level, another risk issue for induration of the arteries and heart condition.
- High blood pressure, smoking, high cholesterol, elevated triglycerides, obesity, diabetes and lack of exercise jeopardize the function of the major heart arteries and are particularly threatening to women’s health.
Key Q&A
- What is atherosclerosis?Often brought up as “hardening of the arteries,” induration of the arteries happens once your arteries slim and settle down versatile as a result of steroid alcohol, fatty substances, cell waste products, calcium and fibrin—collectively called plaque—collect on their inner walls. The arteries respond to the buildup by becoming inflamed. This causes connective tissue to create and different cells to gather within the affected areas, additional narrowing the artery. Atherosclerosis may be a sort of induration of the arteries, that may be a general term for the natural hardening of your arteries that happens with age.
- What causes plaque to build up?We don’t know. Some consultants assume plaque accumulates in places wherever the inner layer of associate artery is broken, probably by elevated steroid alcohol levels, elevated lipoid levels, elevated blood glucose, high blood pressure and cigarette smoke. Smoking particularly accelerates the event of induration of the arteries moreover as increasing pressure level and proscribing the quantity of gas the blood provides to the body. Diabetes is additionally a serious risk issue, and stress has also been implicated, although its exact association with heart disease has not been determined. There are genetic factors that incline people to early induration of the arteries.
- Will I know I have atherosclerosis by recognizing the symptoms?Not necessarily. Often the malady progresses for a protracted whereas before complications or symptoms arise. However, there area unit some conditions which will hint at associate induration of the arteries designation, including chest pain, or angina. However, it’s calculable that common fraction of girls World Health Organization die suddenly from coronary heart condition had no previous symptoms. Therefore it’s vital that you just get screened for upset risk factors and treated as applicable as a result of looking forward to symptoms to develop could also be too late.
- What can I do to prevent atherosclerosis?Changing your habits remains the only handiest thanks to stop the malady from progressing. Changing your diet to at least one low in saturated fat and steroid alcohol helps scale back high blood steroid alcohol, a primary explanation for induration of the arteries. A moderate amount of the healthier polyunsaturated and monounsaturated fats such as in fish, nuts and olive oil may be helpful but be aware of total calories consumed per day. Eating less sugar and eating a diet enriched in fruits, vegetables and fiber should also help you lose weight. If you’re overweight, losing weight will facilitate lower blood steroid alcohol and is that the handiest modus vivendi thanks to scale back high pressure level, another risk issue for induration of the arteries and heart condition. You also can benefit from exercise.
- Is atherosclerosis dangerous?Yes! As the malady progresses, it will utterly clog arteries, cutting off blood flow. This is particularly dangerous in arteries close to the brain, the heart or other vital organs. Completely or nearly blocked blood flow to the heart can lead to a heart attack and kill muscle cells in the heart. The result is permanent heart damage. Plaque may also break loose suddenly and travel through the bloodstream to your brain or heart, causing a stroke or a heart attack.
- Which arteries are most at risk for atherosclerosis?Although atherosclerosis can affect medium and large arteries anywhere in your body, those going to your brain (carotid), heart (coronary) and legs (femoral or iliac) are most at risk.
- How quickly does atherosclerosis occur?While induration of the arteries generally progresses gradually—sometimes even beginning in childhood—you area unit most in danger once blood vessel blockage builds up quickly, completely closing off an artery. This can happen if plaque ruptures and a clot forms.
- Does my risk increase as I age?Yes! Prior to climacteric, women are somewhat protected from heart disease, in part, by estrogen produced by the ovaries. The body’s own natural estrogen helps keep your arteries free from plaque by improving the ratio of LDL (low-density lipoprotein) and HDL (high-density lipoprotein) cholesterol. It additionally will increase the quantity of cholesterol, which helps clear LDL cholesterol—the kind that most contributes to plaque buildup—from the bloodstream. However, supplemental steroid or steroid medical aid isn’t counseled once climacteric to stop against induration of the arteries and heart condition. Also, if you’ve got a case history of early heart condition or if you’ve got polygenic disorder or smoke, you are at risk for heart disease even before menopause.Although risk increases with age, atherosclerosis is a process that develops over years, so don’t put off making lifestyle changes until you are older because it may be too late. It is vital to begin with wholesome habits in youth and time of life to stop complications later in life. Adults with even one major risk factor for heart disease by the age of 50 have an increased lifetime risk of cardiovascular disease and shorter median survival compared to adults with no risk factors.



