Facts of Endometriosis
Overview
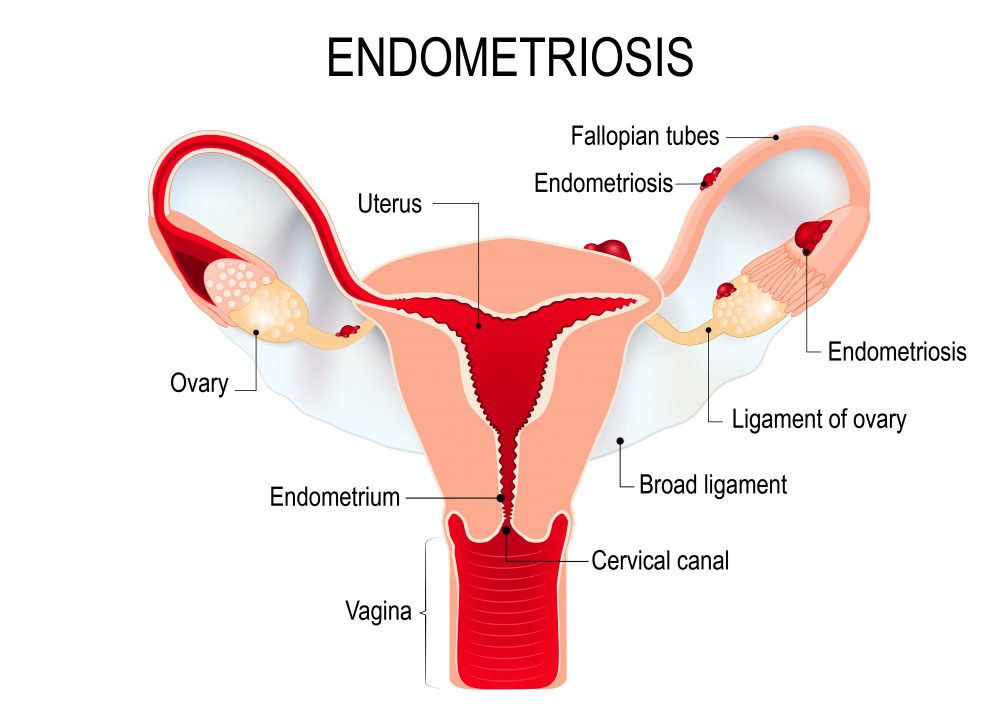
Endometriosis may be a noncancerous condition during which tissue the same as the mucous membrane (uterine lining) grows outside your womb and adheres to alternative structures, most ordinarily within the pelvis, such as on the ovaries, bowel, fallopian tubes or bladder. Rarely it implants in other places, such as the liver, lungs, diaphragmand surgical sites.
It is a common cause of pelvic pain and infertility. It affects about 5 million women in the United States.
Historically thought of as a disease that affects adult women, endometriosis is increasingly being diagnosed in adolescents, as well.
The most common symptoms are painful menstrual periods and/or chronic pelvic pain.
Others include:
- Diarrhea and painful bowel movements, especially during menstruation
- Intestinal pain
- Painful intercourse
- Abdominal tenderness
- Backache
- Severe menstrual cramps
- Excessive menstrual bleeding
- Painful urination
- Pain in the pelvic region with exercise
- Painful pelvic examinations
- Infertility
It is important to understand that other conditions aside from endometriosis can cause any or all of these symptoms and other causes may need to be ruled out. These include, but are not limited to, interstitial cystitis, irritable bowel syndrome, inflammatory bowel disease, pelvic adhesions (scar tissue), ovarian masses, uterine abnormalities, fibromyalgia, malabsorption syndromes and, very rarely, malignancies.
When endometriosis tissue grows outside of the uterus, it continues to respond to hormonal signals—specifically estrogen—from the ovaries telling it to grow. Estrogen is the hormone that causes your uterine lining to thicken each month. When estrogen levels drop, the lining is expelled from the uterus, resulting in menstrual flow (you get your period). But unlike the tissue lining the uterus, which leaves your body during menstruation, endometriosis tissue is essentially trapped.
With no place to travel, the tissue bleeds internally. Your body reacts to the internal bleeding with inflammation, a process that can lead to the formation of scar tissue, also called adhesions. This inflammation and therefore the ensuing connective tissue might cause pain and alternative symptoms.
Recent analysis conjointly finds that this misplaced mucosa tissue might develop its own blood provide to assist it proliferate and nerve provide to speak with the brain, one reason for the condition’s severe pain and the other chronic pain conditions so many women with endometriosis suffer from.
The type and intensity of symptoms vary from fully disabling to delicate. Sometimes, there are no symptoms the least bit, significantly in girls with supposed “unexplained physiological state.”
If your pathology leads to scarring of the generative organs, it’s going to have an effect on your ability to induce pregnant. In fact, thirty to forty % of girls with pathology ar sterilised. Even mild endometriosis can result in infertility.
Researchers do not know what causes pathology, but many theories exist. One suggests that retrograde menstruation—or “reverse menstruation”—may be the main cause. In this condition, menstrual blood doesn’t flow out of the cervix (the opening of the uterus to the vagina), but, instead, is pushed backward out of the uterus through the fallopian tubes into the pelvic cavity.
But as a result of most ladies expertise some quantity of retrograde menstruationwithout developing pathology, researchers believe something else may contribute to its development.
For example, endometriosis could be an immune system problem or local hormonal imbalance that enables the endometrial tissue to take root and grow after it is pushed out of the uterus.
Other researchers believe that in some girls, certain abdominal cells mistakenly turn into endometrial cells. These same cells are the ones responsible for the growth of a woman’s reproductive organs in the embryonic stage. It’s believed that one thing within the woman’s genetic makeup or one thing she’s exposed to within the setting in later life changes those cells in order that they develop into mucosa tissue outside the uterus. There’s also some thinking that damage to cells that line the pelvis from a previous infection can lead to endometriosis.
Some studies show that environmental factors may play a role in the development of endometriosis. Toxins in the environment such as dioxin seem to affect reproductivehormones and immune system responses, but this theory has not been proven and is controversial in the medical community.
Other researchers believe the endometrium itself is abnormal, which allows the tissue to break away and attach elsewhere in the body.
Endometriosis might have a genetic link, with studies finding an increase in risk if your mother or sister had the disorder. No specific genetic mutation has been clearly linked with the disease.
Diagnosis
Gynecologists and reproductive endocrinologists, gynecologists who specialize in infertility and hormonal conditions, have the most experience in evaluating and treating endometriosis.
The condition can be very difficult to diagnose, however, because symptoms vary so widely and may be caused by other conditions.
Among the ways doctors diagnose the disease are:
Laparoscopy. Currently, laparoscopy is the gold standard for the diagnosis of endometriosis and is commonly used for both diagnosis and treatment. Performed under general anesthesia, the surgeon inserts a miniature telescope called a laparoscope through a small incision in the navel to view the location, size and extent of abnormalities (such as adhesions) in the pelvic region.
However, just exploring through the endoscope cannot diagnose deep pathology sickness, in which the endometrial tissue is hidden inside adhesions or underneath the lining of the abdominal cavity. More intensive dissection is required to diagnose and treat this kind of sickness.
Many women have a combination of both deep and superficial (in which the endometrial tissue can be easily seen) endometrial disease.
Peritoneal tissue biopsy. During the laparoscopy, the doctor may remove a tiny piece of peritoneal tissue (the inner layer of the lining of the abdominal cavity) or other suspicious areas to help establish the diagnosis of endometriosis. This is recommended by the American College of Obstetricians and Gynecologists (ACOG), which notes that only an experienced surgeon familiar with the appearance of endometriosis should rely on visual inspection alone to make the diagnosis. A biopsy, however, isn’t necessary to diagnose pathology, and a negative biopsy does not rule out the presence of this disease in other areas within the abdomen.
Ultrasonography, MRI and CT scan. An ultrasound uses sound waves to visualize the inside of your pelvic region, while an MRI uses magnets and a CT scan uses radiation. While these tests can occasionally suggest endometriosis, particularly ovarian endometriotic cysts called “endometrioma,” or rule out other conditions, none can definitively confirm the condition.
At this point, there is no established noninvasive method to diagnosis endometriosis, which is frustrating for both women and their health care providers.
Pelvic exam. Your doctor will perform a physical examination, including a pelvic exam, to aid in the evaluation. The examination won’t diagnose pathology however might permit your doctor to feel nodules, areas of tenderness or plenty on the ovaries which will recommend pathology.
Medical history. A detailed medical history may offer your health care professional the earliest clues in making the correct diagnosis.
Treatment
There is no universal cure for endometriosis. However, there are a number of options available for treating and managing the disease after diagnosis. They represent four categories: medical, surgical, different treatments and physiological state.
- Medical. The foremost common medical therapies for pathology ar nonsteroidal anti-inflammatories (NSAIDs), secretion contraceptives (in oral, patch, and intrauterine or injectable applications) and different secretion regimens, such as GnRH agonists (gonadotropin-releasing hormone drugs).
- Non-steroidal anti-inflammatories (NSAIDs). These medicine, like isobutylphenyl propionic acid, NSAID and analgesic, are often the first step in controlling endometriosis-related symptoms. They may be used long-term in a non-pregnant patient to manage symptoms, in part because they are effective at reducing implantation, are cheaper and easier to use than other options and have fewer side effects than hormonal treatments. However, some patients might expertise severe channel upset from these agents, significantly if they’re administered for prolonged periods and at high doses. They are simpler once taken before pain starts.
- Contraceptive hormones (birth control pills). This option conjointly prices less and has fewer aspect effects than different secretion treatment choices and will be suggested presently when identification. Birth control pills stop ovulation, thus suppressing the effects of estrogen on endometrial tissue. In most cases, ladies taking secretion contraceptives have a lighter and shorter amount than they did before taking them. Often physicians can advocate mistreatment contraception pills ceaselessly as opposition cyclically to eliminate regular menstrual blood, which can be the cause of increased pain in some women with endometriosis.
- Medroxyprogesterone (Depo-Provera). This injectable drug, usually used as birth control, effectively halts menstruation and the growth of endometrial tissue, relieving the signs and symptoms of endometriosis. Side effects include weight gain, depressed mood and abnormal uterine bleeding (breakthrough bleeding and spotting), as well as a prolonged delay in returning to regular menstrual cycles, which can be of concern to women who want to conceive.
- Gonadotropin Releasing Hormone Drugs (GnRH agonists). These drugs block the production of ovarian-stimulating hormones, which prevents menstruation and lowers estrogen levels, thus causing endometrial implants to shrink. GnRH agonists sometimes result in pathology remission throughout treatment and typically for months or years after. However, GnRH agonists have side effects, including menopausal symptoms like hot flashes, vaginal dryness and reversible loss of bone density. Add-back endocrine medical aid, which generally consists of an artificial progestin (progestin) administered alone or together with a low-dose sex hormone, is typically prescribed along with GnRH agonists to alleviate these side effects.
- Danazol. This fruitful endocrine could be an artificial type of a male endocrine (androgen) and is obtainable as Danocrine. It is wont to treat pathology and works by directly suppressing mucous membrane tissue and suppressing gonad endocrine production. A woman taking danazol can usually not release or get regular periods. Side effects might embody weight gain, hair growth and inflammatory disease, among others. Some of the side effects are reversible. Danazol is usually given for 6 to 9 months at a time. Danazol isn’t a contraceptive agent, and it’s essential that any girl taking this drug conjointly use a barrier contraceptive (condoms, diaphragm, IUD) if she is sexually active.
- Progestin-containing intrauterine device. Several studies have shown that Associate in Nursing preventative (IUD) containing an artificial sort of progestin (progestin) also can scale back the painful symptoms and extent of malady related to pathology. If effective, the IUD can be left in the uterus for three to five years and can be removed if a woman wants to conceive. There ar presently 3 FDA-approved brands—Mirena, Skyla, and Liletta—and each has different characteristics; Mirena can be left in place the longest. It should not be used in women with multiple sexual partners, those with an abnormal uterus (fibroids) or those with prior sexually transmitted disease. Side effects include cramping and breakthrough bleeding.
- Aromatase inhibitors. This category of medicine inhibits the actions of 1 of the enzymes that forms sex hormone within the body and might block the expansion of pathology. It is necessary to grasp that this category of medicine isn’t approved to be used within the treatment of pathology by the U.S. Food and Drug Administration; it is under investigation. Side effects embody hot flushes, bone loss and the potential for increased risk of birth defects if a woman conceives while taking these medications and remains on them. Their use should be limited to women participating in research trials or after obtaining written consent from a physician who is thoroughly familiar with this class of drugs.
- Surgical. The goal of any surgical procedure should be to remove endometriotic tissue and scar tissue. Hormonal therapies could also be prescribed along side the a lot of conservative surgical procedures.Surgical treatments range from removing the endometrial tissues via laparoscopy to removing the uterus, called a hysterectomy, often with the ovaries (called an oophorectomy). Surgery classified as “conservative” removes the mucous membrane growths, adhesions and scar tissue associated with endometriosis without removing any organs. Conservative surgery could also be through with a endoscope or, if necessary, through an abdominal incision.
- Laparoscopy. During a laparoscopy, an outpatient surgery also referred to as “belly-button surgery,” the surgeon views the inside of the abdomen through a tiny lighted telescope inserted through one or more small incisions in the abdomen. From there, the physician might destroy mucous membrane tissue with electrical, ultrasound-generated or laser energy or by cutting it out. There is a risk of connective tissue, which could lead to infertility, making pain worse, or damaging other pelvic structures. Surgery to get rid of pathology involving the ureters and viscus is particularly complicated and needs a high degree of surgical ability.
- Laparotomy. A laparotomy is similar to a laparoscopy but is more extensive, involving a full abdominal incision and a longer recovery period.
- Hysterectomy. During a hysterectomy, your uterus is removed. This leaves you infertile. Hysterectomy alone may not eliminate all endometrial tissue, however, because it can’t remove tissue outside of the uterus or ovaries. Additionally, surgery to remove the uterus may not relieve the pain associated with endometriosis.
- Oophorectomy. Removing the ovaries with the uterus improves the likelihood of successful treatment with hysterectomy because the ovaries secrete estrogen, which can stimulate growth of endometriosis. It also renders you infertile, however.
If you wish to preserve your fertility, discuss other treatment options with your health care professional and consider seeking a second opinion.
There has solely been one comparative study of medical and surgical therapies to check that approach is healthier. This trial incontestible improved outcomes with GnRH agonist and add-back medical aid alone or when surgery compared to surgery alone. Each approach has advantages and disadvantages. Often, your set up of care are a mixture of treatments with medical medical aid counseled either before or when surgery.
- Alternative treatments. Alternative treatments for relieving the painful symptoms of endometriosis include traditional Chinese medicine, nutritional approaches, exercise, yoga, homeopathy, acupuncture, allergy management and immune therapy.While some health care professionals may tell you these different ways to seeking pain relief from pathology ar a waste of your time, others might encourage you to do different strategies of pain relief as long as they are not harmful to your condition. Either way, discuss any choices you would like to do along with your health care skilled. Also keep in mind that while these options may help relieve the pain of endometriosis, they won’t cure the condition. Few if any alternative treatments have undergone rigorous scientific evaluation.
- Pregnancy. whereas it cannot be thought of a “treatment” for pathology, gestation might relieve endometriosis-related pain, an improvement that may continue after the pregnancy ends.Health care professionals attribute this pregnancy-related relief to the hormonal changes of pregnancy. For example, organic process and expelling stop throughout gestation, and it’s menstruation that triggers the pain of endometriosis.Plus, endometrial tissue typically becomes less active during pregnancy and may not be as painful or large without hormonal stimulation. However, in several cases, once the pregnancy and breastfeeding end and menstruation returns, symptoms also return.
If pathology has caused physiological state, you have got many treatment choices, as well as surgery, medication to stimulate organic process, typically administered with intrauterine insemination or in vitro fertilization. The appropriate approach would be based on the results of a complete evaluation including an assessment of the male partner. In general, medicines that suppress the painful symptoms of pathology, such as GnRH agonists, oral contraceptives and danazol, do not improve the likelihood of pregnancy. The only doable exception would be that the utilization of a course of GnRH agonists before in vitro fertilization might improve outcomes in bound pathology patients, according to several recent studies.
Prevention
There is no known way to prevent endometriosis. However, some health care professionals believe there might be a certain level of protection against the disease if you begin having children early in life and have more than one child.
Additionally, you may prevent or delay the development of endometriosis with an early diagnosis and treatment of any menstrual obstruction, a condition in which a vaginal cyst, vaginal tumor or other growth or lesion prevents endometrial tissue from leaving your body during menstruation.
There also is some evidence that long-term birth control pill users are less likely to develop endometriosis.
Facts to Know
- Endometriosis is a noncancerous condition that affects about 5 percent of reproductive-age women.
- About 5 million women in the United States have been diagnosed with endometriosis.
- Endometriosis develops once cells almost like the endometrium—or female internal reproductive organ lining—grow outside the female internal reproductive organ and stick with different structures, most typically the ovaries, bowel, fallopian tubes or bladder. Endometrial tissue might migrate outside of the cavity to distant components of the body. Researchers aren’t sure what causes this condition.
- Symptoms of pathology will vary from gentle pain to pain severe enough to interfere with a woman’s ability to guide a traditional life. Other symptoms include heavy menstrual bleeding, cramping, diarrhea and painful bowel movements during menstruation, and painful intercourse. However, you’ll have the sickness and knowledge none of those symptoms.
- A endoscope is often accustomed diagnose and treat pathology. Laparoscopy permits a Dr. to look at abnormalities within the girdle region via a miniature telescope inserted through the wall, usually through the navel. While this can be the most effective technique of identification offered, it doesn’t rule out endometriosis just because the doctor doesn’t see any endometrial tissue.
- Hormonal changes that occur during pregnancy can temporarily halt the painful symptoms of endometriosis since menstruation stops and estrogen levels drop.
- There is no cure for endometriosis. Treatment options include minor and major surgery and medical therapies, including hormonal contraceptives and other hormonal drugs, such as GnRH (gonadotropin-releasing hormone) agonists, that limit the estrogen release that stimulates endometrial tissue growth.
- There is some proof that a case history of pathology might contribute to your chance of developing this sickness. If you have got a mother or sister WHO is battling pathology or has been diagnosed with it, your risk of developing the sickness is above somebody with no family history.
Key Q&A



