Information about Fibroids
Overview
Fibroids are noncancerous masses of muscular tissue and collagen that can develop within the wall of the uterus. They are the most common benign tumor in premenopausal women. By the time girls square measure fifty years recent, eighty % can have fibroids, but only 20 percent of women with fibroids will have any symptoms.
You may hear your health care skilled decision fibroids by different terms as well as female internal reproductive organ leiomyomas, fibromyomas, fibromas, myofibromas and myomas. They can be small or quite large.
While fibroids will cause a spread of symptoms, they will not cause any symptoms at all—so you’ll not even understand you’ve got one. Heavy hemorrhage is that the most typical symptom related to fibroids and therefore the one that sometimes prompts a lady to create a briefing together with her health care skilled. You may learn you have one or more fibroids after having a pelvic exam.
Fibroids may cause a range of other symptoms, too, including pain, pressure in the pelvic region, abnormal bleeding, painful intercourse, frequent urination or infertility.
What truly causes fibroids to create is not clear, however biology and hormones square measure thought to play an enormous role. Your body may be predisposed to developing fibroids. They seem to grow or shrink betting on sex hormone levels in your body, however researchers do not know why some girls develop them whereas others do not.
Fibroids usually grow slowly during your reproductive years, but about 40 percent of fibroids increase in size with pregnancy.
At menopause, fibroids shrink because estrogen and progesterone levels decline. Using menopausal hormone therapy containing estrogen after menopause usually does not cause fibroids to grow. Growth of a fibroid after menopause is a reason to see your gynecologist to make sure nothing else is causing the growth.
Progesterone and growth hormone are other hormones that may stimulate a fibroid’s growth once it has already formed.
A variety of treatments exist to remove fibroids and relieve symptoms. If you learn you have fibroids but aren’t experiencing symptoms, you usually won’t need treatment.
Who Is at Risk for Fibroids?
Your risk for developing fibroids increases with age. African-American women are more likely than Caucasian women to have them, and they are more likely to develop fibroids at a younger age. If women in your family have already been diagnosed with fibroids, you have an increased risk of developing them. You may also be at an increased risk if you are obese or have high blood pressure.
Types of Fibroids
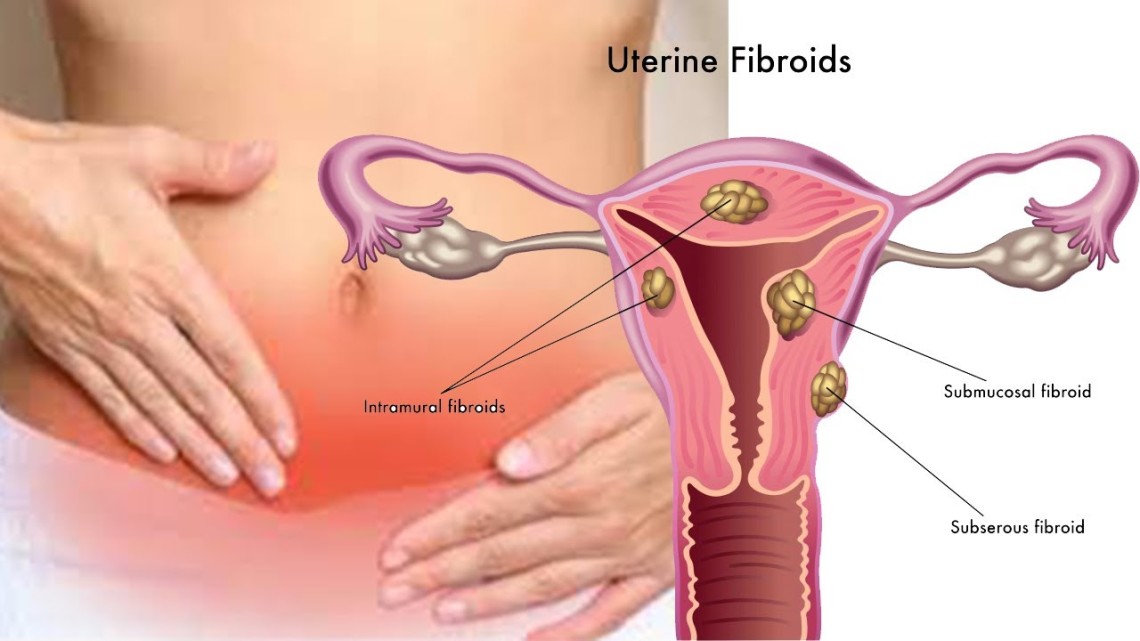
Fibroids form in different parts of the uterus:
- Intramural fibroids are confined within the muscle wall of the uterus and are the most common fibroid type. They expand, which makes the uterus feel larger than normal. Symptoms of intramural fibroids may include heavy menstrual bleeding, pelvic pain, back pain, frequent urination and pressure in the pelvic region.
- Submucosal fibroids grow from the uterine wall into the uterine cavity. They can cause heavy menstrual bleeding with associated bad menstrual cramps and infertility.
- Subserosal fibroids grow from the uterine wall to the outside of the uterus. They can push on the bladder or bowel causing bloating, abdominal pressure, cramping and pain.
- Pedunculated fibroids grow on stalks out from the uterus or into the uterine cavity, like mushrooms. If these stalks twist, they can cause pain, nausea or fever, or extremely rarely can become infected.
Diagnosis
More than half girls United Nations agency have fibroids ne’er expertise symptoms. When fibroids square measure symptom-free, they typically do not need treatment. But even little fibroids will cause significant or longer-than-normal expelling hemorrhage and important pain. Fibroids may also contribute to infertility.
The three most common symptoms caused by fibroids are:
- Abnormal uterine bleeding. The most common hemorrhage abnormality is significant expelling hemorrhage—menstrual bleeding that’s too significant or long. Normal menstrual periods last four to seven days. If you’ve got abnormal hemorrhage from fibroids, your periods square measure seemingly to last longer or is also heavier. Instead of changing a pad or tampon every four to six hours, you may have to change one every hour and find that your periods greatly interfere with your daily activities. You may conjointly expertise breakthrough hemorrhage, or hemorrhage that happens between periods.
- Pelvic pressure. You may experience pressure in the pelvic region. Many women with fibroids have an enlarged uterus. Pelvic pressure may be caused by either the increased size of your uterus or from the location of one fibroid in particular. Health care professionals usually describe the size of a uterus with fibroids in the same terms used for someone who is pregnant, such as a “12-week-size fibroid uterus.”You may also expertise pressure on areas close to your pelvis, including your bowel or bladder. Pressure against these structures can lead to difficulty or pain with bowel movements and constipation or increased urinary frequency and incontinence. Conversely, you may not be able to empty your bladder because the fibroid is in the way or you may get recurrent urinary tract infections.
- Reproductive problems. Fibroids also are associated with reproductive problems, depending on the number of fibroids present in the uterus and on their size and specific location. While having fibroids will cause complications with physiological condition, most don’t have any impact. Fibroids in a uterus do not create a high-risk pregnancy. The risks from fibroids could embody the next risk of miscarriage, sterility, childbed and labor complications.
Symptoms caused by fibroids is almost like variety of different symptoms caused by a spread of different conditions, as well as generative cancers, sexually transmitted infections and gut and bladder disorders. So, if you are having any unusual symptoms, be sure to make an appointment to discuss them with your health care professional.
The first step in designation fibroids is typically a girdle examination and a comprehensive anamnesis performed by your health care skilled. He or she may be able to feel the fibroids in your uterus during the exam, because fibroids can make the uterus feel enlarged or irregular. If the female internal reproductive organ is enlarged enough, it may also be felt abdominally above the pubic bone.
To confirm the diagnosis, even if nothing is felt, your health care professional may recommend one or more diagnostic tests.
Ultrasound is perhaps the foremost common choice accustomed ensure the diagnosing. It is necessary to notice that imaging could realize terribly little fibroids that do not cause any medical issues, wouldn’t be felt on physical examination and may not be causing symptoms.
If you’ve got significant or prolonged hemorrhage or have had multiple miscarriages, your health care professional may recommend a more involved examination of your uterine cavity to see if you have a submucous fibroid, which might go undetected on a regular ultrasound. The assessment can be performed in one of four ways:
- Magnetic resonance imaging (MRI). MRI uses a magnet (not x-ray) to make an image of the uterus. It is the most accurate way to determine the positions, sizes and number of fibroids you have.
- Hysteroscopy. The uterus is expanded with a liquid or gas, and a hysteroscope (a small telescope) is inserted directly into the uterus through the vagina and cervix enabling your health care professional to see your entire uterus. Fibroids within the uterine cavity can also be removed during this surgery.
- Saline-infused sonography. A saline solution is injected into your uterus, and ultrasound is used to visualize the uterine cavity. Also known as hysterosonography, this test is most useful in women who have prolonged or heavy menstrual bleeding but normal ultrasound results.
- Hysterosalpingography (HSG). A dye that shows up on an X-ray is injected into your uterus, enabling your health care professional to evaluate the structure of your uterine cavity and look for any abnormalities in the uterus or fallopian tubes. This test may be recommended if you are trying to get pregnant to check if your tubes are open, but it is not very accurate when looking for fibroids..
Imaging tests, such as computed tomography (CT), may also be ordered but is not very accurate for the diagnosis of fibroids.
If you’re experiencing abnormal duct hemorrhage as a results of fibroids, your health care skilled might want to conduct different blood tests, as well as an entire blood count, to rule out other conditions.
Treatment
If you aren’t experiencing symptoms caused by your fibroids, you usually do not need any treatment. And, if your symptoms aren’t severe, you may decide you can put up with them. This may be especially true if you’re close to menopause—a time when fibroids shrink and symptoms resolve. It’s important to discuss all your options with your health care professional and consider his or her recommendations when weighing your treatment options.
You may need to do the “watch and wait approach,” wherever your health care skilled sporadically evaluates the dimensions of your fibroids throughout routine girdle exams and discusses what quantity discomfort you’re feeling or how the symptoms may be disrupting your lifestyle.
Fibroids that do not cause symptoms seldom want medical aid unless they get large enough to have an effect on different structures within the girdle space, like the kidneys or the epithelial duct (the tube that drains the kidney to the bladder).
The need for treatment and therefore the kind of treatment you select depends on the dimensions and position of the fibroids, moreover as any symptoms they are inflicting, your age and whether or not you want to have children in the future. Even with a range of treatment choices out there, new fibroids might grow back to some extent within the years following most treatments. The need for repeat treatments ranges from ten % to twenty five %, counting on the amount and sizes of the fibroids at the start treated. No treatment—except hysterectomy—can guarantee that new fibroids will not grow. The more fibroids you have, the more likely you are to have a recurrence after treatment.
If bleeding is your major symptom, some women opt for managing this symptom with medication before surgery or as a way to delay surgery if they’re close to menopause (because fibroids generally shrink and cause few or no problems after menopause).
Medical Treatment Options for Fibroids
- Oral contraceptives (OCs). While OCs don’t treat fibroids, they’ll be counseled to manage significant injury caused by fibroids or for girls WHO expertise irregular organic process additionally to fibroids. OCs ar the primary treatment possibility for several ladies, often combined with a nonsteroidal anti-inflammatory such as ibuprofen. OCs do not make fibroids grow.
- Intrauterine device (IUD). The levonorgestrel intrauterine device (Mirena), which is usually prescribed for birth control, can help ease the heavy bleeding that accompanies some fibroids. The device will not shrink the fibroids, however, and depending on whether or not the fibroids have distorted the inside of the uterus, it may or may not provide effective birth control. Although the levonorgestrel contraceptive is FDA-approved for significant catamenial injury, it isn’t approved specifically for the treatment of fibroids, so if you are interested in this option, discuss it with your doctor.
- GnRH agonists. Gonadotropin-releasing hormone (GnRH) agonists, including leuprolide (Lupron), nafarelin nasal (Synarel) and goserelin (Zoladex), temporarily shrink fibroids by blocking estrogen and progesterone production; estrogen is thought to stimulate their growth. They are primarily employed in ladies getting ready to biological time or to shrink fibroids before removing them surgically or to correct anemia caused by significant injury related to fibroids. GnRH agonists ar thought of a short-run treatment as a result of they block endocrine production by the ovaries, thus triggering menopausal symptoms caused by estrogen depletion, such as hot flashes, vaginal dryness and bone loss. The usual course of treatment is 3 to 6 months, and it may be combined with estrogen and/or progesterone hormones to minimize menopausal symptoms. Once this medication is stopped, fibroids usually grow back to near pretreatment size or larger within several months.
- Antifibrinolytic medicines. Antifibrinolytic medicines ar medication that facilitate slow catamenial injury by serving to blood to clot. The drug tranexamic acid (Lysteda) is FDA-approved for significant catamenial injury. Rare side effects include headaches, muscle cramps, or pain. Antifibrinolytic medicines don’t have an effect on your possibilities of changing into pregnant. They should not be crazy secretion contraception while not previous approval from a health care skilled because the combination will cause blood clots. Antifibrinolytic therapies ar comparatively new and expensive—and typically not lined by insurance. Check with your insurer if that is a concern.
Minimally Invasive Treatment Options
- Uterine artery embolization (UAE). UAE is a procedure that involves placing a small catheter (a thin tube) into an artery in the groin and guiding it via X-rays to the arteries in the uterus. Then, tiny particles similar in size to grains of sand are injected through the catheter and into the artery. As they move toward the uterus, they obstruct the blood supply to the fibroids. Without an adequate blood supply, the fibroids shrink. The uterus is spared, however, because an alternate blood supply develops to support it.UAE takes about one hour to perform and is typically performed by an interventional radiologist. It usually requires a one-night hospital stay. Most women are back to their normal activities in seven to 10 days.While this treatment option leaves your uterus intact, it’s not recommended for women who wish to become pregnant within the future.Potential complications include fever, passage of small pieces of fibroid tissue through the vagina after the procedure, allergic reaction and hemorrhage. Complications can also occur if blood supply to the ovaries or other organs becomes compromised.
- Endometrial ablation. This technique is employed to treat tiny fibroids inside the womb or significant periods caused by fibroids. Endometrial ablation uses electrical energy, heat or cold to destroy the lining of the uterus. It is performed on AN patient basis and is simply offered as a treatment choice to ladies WHO have finished childbearing. It is not counseled for girls WHO would like to preserve fertility. However, employing a reliable variety of birth prevention once having ablation is very important.
Surgical Options for Fibroids
- Hysterectomy. An ablation offers the sole real cure as a result of it utterly removes the female internal reproductive organ.However, ablation is operation, requiring between 2 and eight weeks of recovery, counting on the sort of surgery performed. Hospital stays and recovery times will vary supported the sort of procedure used and also the extent of the surgery performed. Because your uterus and, sometimes, your ovaries, are removed, it is not an option if you want to become pregnant. If your ovaries do not need to be removed, you may want to keep your ovaries to maintain estrogen production.If you and your health care professional decide that a hysterectomy is the best choice for you, you may have several options about how the procedure is performed:
- Abdominal hysterectomy, in which the uterus is removed through an incision in the abdomen. It is generally used for large pelvic tumors or suspected cancer because this procedure allows the surgeon to see and manipulate the pelvic organs more easily.
- Vaginal hysterectomy, in which the uterus is removed through the vagina.
- Laparoscopically hysterectomy, in which a surgeon uses a laparoscope (a small telescope) inserted through the abdomen to see inside your pelvis. Laparoscopic hysterectomy is less invasive than an abdominal hysterectomy, but more invasive than a vaginal hysterectomy.
- Robotic-assisted laparoscopic hysterectomy, in which a robotic system assists in removal of the uterus in a laparoscopic hysterectomy. It may be helpful with some patients because of the flexibility it allows, but it also adds to the time and cost of the procedure.
- Myomectomy. This procedure removes only the fibroids, leaving the uterus intact, which can preserve fertility. The procedure is performed through an incision in the abdomen (a laparotomy), which requires general anesthesia, or by laparoscopy, which uses a few small incisions to insert an operative camera and surgical instruments. Robotic myomectomy is a variation of laparoscopic myomectomy during which the surgical procedure is aided with a surgical robot. A full recovery from laparotomy can take up to six weeks and two weeks from laparoscopy. Your health care skilled can suggest that procedure to use supported the dimensions of the fibroids, as well as whether they are superficial or deep (which is too difficult for laparoscopy).A hysteroscopic myomectomy is performed through the vagina and requires no incision. It is applicable just for girls whose fibroids area unit within the mucosa cavity. With this procedure, fibroids are removed using an instrument called a hysteroscopic resectoscope, which is passed through the vagina into the uterine cavity. A wire loop carrying electrical current is then wont to shave off the fibroid.Blood loss may be slightly greater with a myomectomy than with hysterectomy, but surgeons use tourniquets and medications to regulate blood loss, so that transfusion rates are no greater than with hysterectomy.
- Magnetic resonance guided focused ultrasound. A more recent fibroid treatment option, magnetic resonance guided focused ultrasound surgery (MRgFUS or FUS) is a noninvasive treatment that takes place inside an MRI machine. The machine guides the treatment, which consists of multiple waves of ultrasound energy that go through the abdominal wall and destroy the fibroid. The procedure requires sedation but is usually performed on an outpatient basis. In the weeks and months that follow, fibroids shrink and heavy menstrual flow decreases. Pregnancy is not counseled once FUS, but it is possible to become pregnant following the procedure.
- Radiofrequency ablation. Acessa is a new FDA-approved laparoscopic surgical procedure that uses radiofrequency energy to destroy fibroids. The energy heats the fibroid tissue and kills the cells, that area unit then reabsorbed by the vascular system, decreasing fibroid size and symptoms. The procedure is minimally invasive, performed under ultrasound guidance during an outpatient pelvic laparoscopy. The early results regarding the safety and effectiveness of Acessa are good. On average, women returned to normal activities in nine days. The long-term risk of fibroid recurrence has not yet been determined, though a 12-month follow-up in one study showed good results.
Prevention
Fibroids can’t be prevented. If you are experiencing symptoms, such as heavy bleeding and pelvic pressure, contact your health care professional for an evaluation. If you have a family history of fibroids or have been treated for them in the past, you may want to be examined more frequently or investigate the various management strategies available to treat fibroids.
Facts to Know
- Fibroids are not cancerous and they do not turn into cancer. They are balls of muscular tissue that grow inside the uterus, on the surface of the uterus or in the muscular wall of the uterus.
- Up to 80 percent of women have fibroids, but not all of these women have symptoms. They are most commonly found in women in their 40s and early 50s.
- African-American women are more likely to have fibroids than Caucasian women.
- If there are women in your family who already have been diagnosed with fibroids, you have an increased risk for developing them.
- Fibroids usually grow slowly during the reproductive years, but may increase in size with pregnancy. At menopause, fibroids usually shrink, because estrogen and progesterone levels decline. Estrogen replacement therapy may rarely interfere with this shrinkage after menopause.
- More than half of the women who have fibroids never experience symptoms and require no treatment. In general, the severity of symptoms varies based on the number, size and location of the fibroids.
- The two most common symptoms of fibroids are heavy menstrual bleeding and pelvic pressure. Normal menstrual periods last four to seven days, but if you have fibroids, your periods are likely to last longer. The bleeding might be so heavy that you may need to change your sanitary pads or tampons as often as every hour.
- Fibroids may be associated with a handful of reproductive problems, depending on the number of fibroids in the uterus and their size and specific location. While fibroids can cause complications with pregnancy, most do not have any impact. Fibroids in a uterus do not create a high-risk pregnancy. The risk from fibroids may include a higher risk of miscarriage, infertility, premature labor and labor complications.
- Oral contraceptives (estrogen and progestin and progestin-only) are sometimes recommended to manage heavy bleeding caused by fibroids, but they aren’t used to treat fibroids.
- There are several treatment options available for fibroids, including medication, minimally invasive options and surgical options.
Key Q&A
- How do I know I have fibroids?More than half of all women who have fibroids have no symptoms. If you aren’t experiencing any problems, there’s usually no reason to treat the fibroids. The two most common symptoms of fibroids are heavy menstrual bleeding and pelvic pressure. Normal menstrual periods usually last four to seven days, but if you have fibroids, your periods are likely to last longer.If you have fibroids, the bleeding might be so heavy that you may need to change your sanitary pad or tampons as often as every hour. Bleeding between periods isn’t usually associated with fibroids, but it may occur in rare situations.You may also experience pressure in the pelvic region from an increase in the size of your uterus or from the location of one fibroid in particular. If you notice these symptoms, you should definitely seek a diagnosis from your health care professional.
- Are fibroids hard to diagnose?Not usually. A health care professional should be able to feel some kind of irregularity in your pelvic region during a regular office pelvic exam. If fibroids are suspected, more detailed tests may be conducted to confirm the initial diagnosis. These may include ultrasound, magnetic resonance imagery (MRI), hysteroscopy, saline-infused sonography or hysterosalpingogram (HSG), a test that involves injecting a special dye into the uterus and then taking an X-ray of the area. Ultrasound is the most common option used to confirm the diagnosis, and MRI is the most accurate.
- Does the location of my fibroids really make a difference in how they’re treated?The symptoms you experience may vary depending on where the fibroids are located. However, the ultimate course of treatment for your fibroids will likely depend more on other factors, such as whether you plan to have children or how close to menopause you are. If preserving your fertility is a priority, several options won’t be recommended.
- Is a hysterectomy really the only way I can get rid of my fibroids forever, or at least before I reach menopause?Yes. While other procedures are helpful because the existing fibroids are removed or shrunk, there is no guarantee that new fibroids won’t develop. There are newer surgical procedures, such as myomectomy, robotic myomectomy, magnetic resonance guided focused ultrasound surgery, and radiofrequency ablation (Acessa procedure), that are showing success in treating fibroids while sometimes preserving fertility. Your health care professional will recommend which procedure is best for you.
- Is there anything I can do to protect myself from developing fibroids?Unfortunately, there isn’t. Fibroids appear to affect women mostly in their 30s and 40s. Genetics and hormones appear to play a role in who develops fibroids.
- I’ve heard that estrogen and other hormones can make fibroids grow. Should I avoid taking birth control pills that contain estrogen?No, there is no evidence that oral contraceptives have any effect on fibroid size. In fact, health care professionals prescribe oral contraceptive pills for some women with fibroids to help control the prolonged or excessively heavy blood flow during menstruation.
- Do I need to see a specialist other than my gynecologist to diagnose and treat fibroids?Your gynecologist should have adequate experience in diagnosing fibroids because they are so common. However, some gynecologists may have more experience or better success at treating fibroids. If you’re considering any of the more innovative treatments, whether surgical or medical, make sure you see a practitioner with a strong track record in treating fibroids, and ask about their success rates.
- Are hormone therapy treatments for fibroids dangerous?GnRH agonists are one treatment option for fibroids. This treatment shrinks fibroids by blocking hormone production by the ovaries. Because estrogen production is suppressed temporarily, you will experience menopausal symptoms such as hot flashes and vaginal dryness. Treatment is usually limited to three to six months.
To offset hot flashes and other uncomfortable menopausal symptoms caused by GnRH agonists, your doctor may add estrogen and/or progesterone therapy.
Ask your health care professional to review the risks associated with menopausal hormone therapy and how they may or may not be relevant to your treatment needs for fibroids.



