What is Chronic Obstructive Pulmonary Disease (COPD)???
Overview
Chronic preventive respiratory organ illness (COPD) could be a respiratory organ disorder that generally happens in older adults with a history of smoking. It kills one person every four minutes in the United States and is one of the few causes of death that continues to increase. Today, a lot of ladies than men have COPD, with associate calculable seven million ladies diagnosed with the illness. The prevalence of COPD is increasing among ladies whereas decreasing among men. Plus, a lot of ladies than men die once a year from the illness.
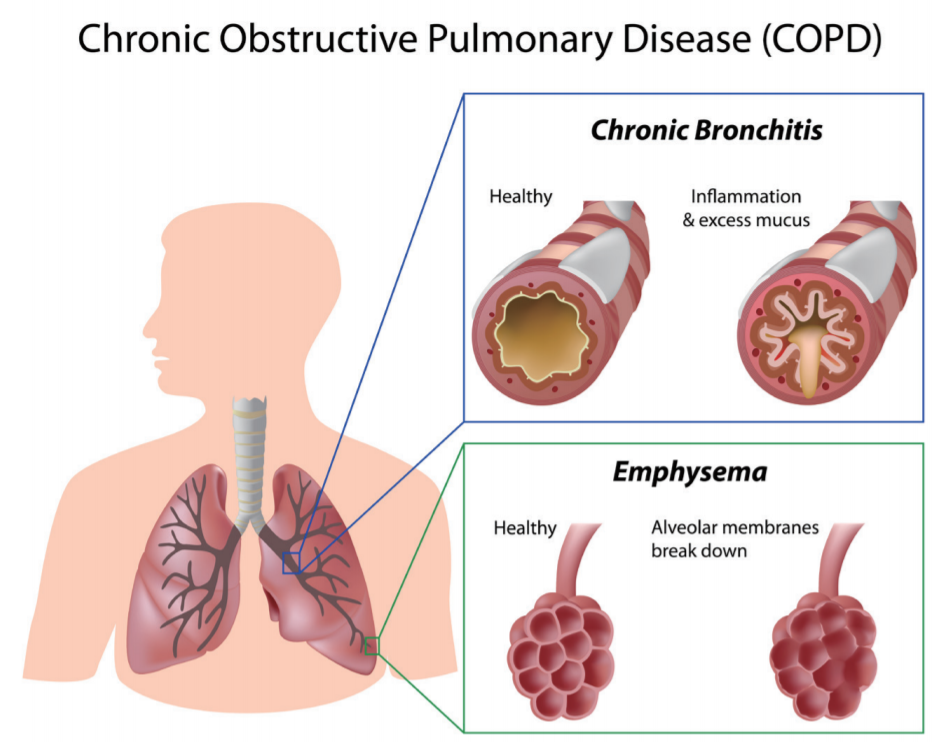
When you have COPD, your airways and therefore the little air sacs within the respiratory organ (alveoli) area unit broken by smoking or different indrawn particles and gases, which cause swelling, or inflammation. Eventually, this damages the lungs making it hard to breathe in and out and difficult for oxygen and carbon dioxide to pass through the air sacs.
Chronic preventive respiratory organ illness wont to be represented as bronchitis oremphysema, however nowadays we all know that each conditions area unit types of COPD. Asthma could be a separate conditions that additionally involves air flow limitation however affects folks of all ages and generally affects those forty and older. In addition, breathing issues in asthma can often be resolved with bronchodilator medication, while the airways with COPD may be only partially opened with medication.
It is possible, however, to have emphysema, bronchitis and asthma all at the same time.
An estimated 14.8 million Americans have been diagnosed with COPD. Although more adults are aware of the disease today than a few years ago (71 percent compared to 65 percent in 2008), a substantial number of people still do not understand the illness, its symptoms and the way it’s managed. In fact, an estimated 12 million people may have COPD and remain undiagnosed.
Although the first reason behind COPD is butt smoking, regarding ten to twenty p.c of these diagnosed—one out of six folks with the disease—have ne’er preserved. Instead, they developed the condition from environmental exposures such as air pollution or work-related fumes, exhaust or dust. Other potential causes embrace low birth weight, vertebrate biological process problems, babyhood infections and genetic factors. Further, close to 100,000 Americans have a genetic condition known as alpha-1 antitrypsin, or AAT deficiency, that has been linked to COPD.
Diagnosis
It is important that you get diagnosed as early in the disease as possible. While there’s no cure for COPD, early and semipermanent treatment could improve symptoms, help you breathe better and reduce the risk of exacerbations (sudden worsening of your symptoms).
Unfortunately, studies find that doctors are not very good at diagnosing COPD in women because they have long considered it a “man’s disease.” If you think you might have COPD, ask your health care skilled to check your respiratory organ perform with spirometry.
Symptoms of COPD could embrace shortness of breath, notably within the morning however eventually throughout the day. You may also have a cough and mucus production. Over time, your symptoms may worsen, particularly when exercising or climbing stairs, for example. You may notice that you’ve cut back on certain activities, because they make you too tired or cause shortness of breath or chest tightness. As the illness gets worse, these symptoms occur even when you’re resting. Other symptoms may include fatigue and morning headaches.
COPD is marked by hyperinflation of the lungs, meaning you can’t exhale all the air you’ve inhaled, so your lungs remain inflated like a balloon. This additionally interferes with what proportion air you’ll be able to inhale, leading to the shortness of breath that is a primary symptom of the disease.
To diagnose COPD, your doctor will take a complete medical history and listen carefully to your lungs before ordering certain tests. These may include:
- Spirometry. This simple test uses a spirometer, which is a machine that checks how well your lungs function and displays the results on a graph. It measures two things:
- Forced vital capacity (FVC), how much air you can exhale after taking in a deep breath.
- Forced expiratory volume (FEV1), how much air you can exhale in one second.
Your doctor can browse the results, assess how well your lungs are working and determine if you have COPD. You are typically diagnosed with COPD if you have an FEV1/FVC ratio less than 70 percent and an FEV1 less than 80 percent of what would be “predicted” based on your age, gender, weight and other parameters.
Spirometry is used not only to confirm your diagnosis, but also to track the progression of your disease over time.
- Other pulmonary tests. You may endure different respiratory organ tests, including one that measures your lung volume, and oximetry, in which a small sensor is clipped to your finger to measure the oxygen level in your blood.
- X-ray. Your doctor may order an X-ray to examine your lungs. However, X-rays are not very good at detecting COPD, so if your doctor does order one, ask why.
- CT scan. Although not required for a diagnosis, your doctor may order a CT scan, particularly to see if you have emphysema.
- Arterial blood gases. This check measures the number of gas and carbonic acid gas in your blood, as well as the acidity (pH) of your blood. As your COPD worsens, carbon dioxide builds up because you have a hard time exhaling.
Once you’re diagnosed, your doctor will classify your disease into one of four grades: mild (GOLD 1), moderate (GOLD 2), severe (GOLD 3), very severe (GOLD 4). The grade helps determine the best treatment regimen.
Exacerbations. Exacerbations are periodic flare-ups of COPD symptoms, such as cough, mucus production and shortness of breath. Although they have a tendency to occur a lot of oft in patients with a lot of severe illness, they can occur at any stage of the disease. They are marked by hyperbolic shortness of breath, greater difficulty trying to breathe out and higher levels of carbon dioxide because of reduced lung function. They generally result in a amendment in your medication and should need hospitalization. A major goal of treatment is to reduce the risk of exacerbations.
Comorbidities. COPD doesn’t just affect your lungs. The inflammation that accompanies the illness, not to mention the chronic, or semipermanent, gas deficiency, will contribute to varied health issues that area unit a lot of prevailing in folks with COPD than in those without the disease. Among them are:
- depression
- diabetes
- heart disease
- high blood pressure
- infections
- lung cancer
- osteoporosis
Two of the most common comorbidities are depression, which affects 28 to 42 percent of those with COPD, and osteoporosis, which is three to five times more common in those with COPD than in those without it. One study found that 68 percent of those aged 50 to 70 with COPD had osteoporosis.
Treatment
The goals of treating COPD area unit to scale back your symptoms and risk of exacerbations, and improve your overall health and exercise tolerance.
COPD is treated with a combination of medication and nonmedical approaches. An important a part of managing COPD, however, includes an honest relationship and open communication together with your doctor, and following your doctor’s instructions.
Nonmedical treatments
- Smoking cessation. If you smoke, you must stop. Continuing to smoke can increase injury to your lungs and worsen your symptoms. Your best chance at success in quitting smoking is to enlist the help of your doctor and to find a support system, either in person, by phone or online. You may also need medication or a nicotine replacement product, like gum or a patch.You may experience some nicotine withdrawal symptoms, because nicotine can be quite addictive. These include sleeplessness, irritability, dizziness, headaches, increased appetite and weight gain. Be patient; symptoms usually peak within two to three days and disappear between a few days to several weeks after quitting.
- Pulmonary rehabilitation. This includes exercises to strengthen the muscles that help you breathe (your diaphragm), as well as regular exercise, such as walking. If there’s no formal pulmonic programme close to you, you must attempt to walk a minimum of twenty minutes each day or till you’re feeling any dyspnea or different symptoms. Studies notice that pulmonic rehabilitation programs will improve your ability to exercise, cut back shortness of breath, improve your quality of life and reduce the amount of medical services you use.
- Nutrition. About a third of people with severe COPD eat too little protein and develop protein-related malnutrition. This may make your COPD worse and increase your risk of death. Talk to your doctor about whether you should take high-calorie nutritional supplements and, if needed, appetite stimulants. You also might consider:
- Eating small, frequent meals with high-protein foods that are easy to fix, such as hard-boiled eggs, peanut butter, chicken breasts, cubes of cheese, cottage cheese and yogurt.
- Resting before meals.
- Taking vitamins (check with your doctor on the best options).
- Education. The more you know about your COPD, the better you may be able to manage it. It is important that you understand what triggers exacerbations, what medications you need and how to use them, how to reduce shortness of breath and how to recognize and treat complications. Education allows you to take a larger role in managing your COPD.
Types of Medications
Several types of medication are used to treat COPD symptoms. In some instances, you may be placed on more than one medication to control your symptoms.
The most commonly used medications are:
Bronchodilators. Bronchodilators work by relaxing your airways so you can breathe easier. They improve each respiratory organ operate (which spirometry measures) and symptoms, can increase your exercise ability and can improve airflow. They may also reduce your risk of exacerbations and hospitalization.
This is important because the more exacerbations you have, the higher your risk of future exacerbations. They may conjointly hasten illness progression, leading to worse lung function more quickly. Thus, bronchodilators are a standard type of COPD treatment. All are inhaled, although they may be delivered via different types of inhalers. Long-acting bronchodilators area unit convenient and more practical at maintaining symptom relief than short-acting therapies.
Inhaled glucocorticoids (also known as inhaled corticosteroids, or ICS)
These medicine might facilitate cut back inflammation from COPD and should cut back exacerbations. They area unit ne’er used as solo medical aid for COPD and are forever prescribed in conjunction with a long medicine, sometimes two, in people with more severe COPD, significant symptoms or repeated exacerbations. They are used to treat asthma. Potential facet effects of ICS embrace thrush, hoarse voice and bruising.
Phosphodiesterase-4 (PDE-4) inhibitor
This class of drug reduces inflammation and may increase airway relaxation. It is generally reserved for those with severe or very severe COPD, particularly those experiencing frequent exacerbations, severely limited airflow and chronic bronchitis.
Inhalers. Most medications for COPD are delivered via inhalers.
There are four main types of inhalers:
- Metered dose inhaler (MDI). With these inhalers, you insert an aerosol canister of medication at the end of a small tube, press down on the canister and breathe in deeply. MDI needs coordination between your hand and breath, and you must be able to take a deep breath. There area unit breath-activated MDIs, which are triggered when you breathe in and may be easier to use. Still, studies find that up to 67 percent of people do not use MDIs properly.
- Dry powder inhaler. With these inhalers, you insert a specific dose of the medication into the device, put the mouthpiece between your lips and breathe in deeply. They are portable and easy to use, but any exposure to moisture can ruin the medicine because it’s a dry powder. You also have to be able to breathe in deeply to get the right dose of medicine.
- Nebulizer. With a nebulizer, the medicine is automatically sent through a mouthpiece. You breathe in through the mouthpiece to get the medicine into your lungs, and out through your nose. For some people, a nebulizer may be the easiest delivery system to use, but it is bulky and requires more time than other types of inhalers.
It is important that you work with your health care professional to find the right inhaler for you and to become comfortable with how it works. If you don’t like the one you’re using, ask about switching. Many inhalers are very effective, but the key is to find one that works for you and that you can use properly. Things such as your age, eyesight and other medical conditions can all affect your ability to use the medicine. Remember: the medication only works if it gets into your lungs.
Vaccinations. Any reasonably respiratory organ infection, as well as a chilly, will result in a COPD exacerbation. You can’t prevent all such infections, but you can protect yourself against pneumococcal pneumonia and the flu with vaccines. So make sure you get a flu vaccine every year. If you are 65 or older, or you have an FEV1 less than 40 percent, you should consider getting a pneumococcal polysaccharide (pneumonia) vaccine.
Rarely Used Medications
There are alternative medications that were once oftentimes wont to treat COPD however ar currently sometimes solely prescribed in restricted circumstances. These drugs include: systemic glucorticoids, which are sometimes used for short-term treatment of exacerbations; mucus-thinning agents, which may benefit people with certain COPD symptoms, but are not widely recommended; and antibiotic medical aid, which can be used on a short basis to treat microorganism infections however is sometimes not required long-run if your COPD is well-controlled.
Other Treatments
- Oxygen. As your condition worsens, you will need supplemental gas medical aid to assist you breathe. Long-term gas medical aid is merely suggested for folks within the advanced stages of COPD WHO have low gas levels within the blood.
- Surgery. Some people with severe COPD may qualify for surgery.
- Lung volume reduction surgery. This type of surgery is performed in folks with severe hyperinflation of the respiratory organ, during which an excessive amount of air remains within the lungs. The doctor removes a part of your respiratory organ to scale back the hyperinflation to boost your respiratory organ perform.
- Lung transplant surgery. Also reserved for those with the most severe stage of COPD. Although it can reduce your symptoms, there is no evidence that lung transplant prolongs your life.
Prevention
The best way to prevent COPD is to never smoke or stop smoking and avoid secondhand smoke. Also avoid exposure to toxic fumes or gases in your home, environment and workplace.
Facts to Know
- Chronic obstructive pulmonary disease (COPD) causes one death every four minutes in the United States and is one of the few causes of death that continues to increase.
- An estimated 14.8 million Americans have been diagnosed with COPD, 7 million of them women. It’s also estimated that another 12 million people may have COPD and don’t know it.
- The prevalence of COPD remains higher in women than men, based on 2011 data from the Centers for Disease Control (CDC).
- When you have COPD, your airways and also the little air sacs within the respiratory organ (alveoli) ar broken by smoking or alternative inhaled particles and gases, which cause swelling, or inflammation. Eventually, this damages the lungs making it hard to breathe in and out and difficult for oxygen and carbon dioxide to pass through the air sacs.
- Chronic obstructive pulmonary disease used to be described as chronic bronchitis or emphysema, but today we know that both conditions are part of COPD.
- Although the primary cause of COPD is cigarette smoking, about 10 to 20 percent of those diagnosed have never smoked. Instead, they developed the condition from environmental exposure such as air pollution or work-related toxins. Other causes embrace your genetic makeup, being small at birth and a history of respiratory infections in childhood.
- Early diagnosis and treatment of COPD is desirable to managing the disease.
- Symptoms of COPD include shortness of breath, particularly in the morning but eventually throughout the day. You may also cough and have mucus production.
- COPD is diagnosed with pulmonary function tests like spirometry; sometimes with X-rays or a CT scan.
- Treatment for COPD includes medications and lifestyle changes, as well as pulmonary rehabilitation.
Key Q&A
- What is COPD?Chronic obstructive pulmonary disease (COPD) is a lung disorder that typically occurs in older adults with a history of smoking. It causes one death every four minutes in the United States and is one of the few causes of death that continues to rise. When you have COPD, your airways and the tiny air sacs in the lung (alveoli) are damaged by smoking or other inhaled particles and gases, which cause swelling, or inflammation. Eventually, this damages the lungs making it hard to breathe in and out and difficult for oxygen and carbon dioxide to pass through the air sacs.
- What causes COPD?The primary cause of chronic obstructive pulmonary disease is cigarette smoking, but it may also be caused by exposure to air pollution and other lung irritants, genetics and, possibly, respiratory infections as a child. There is also a strong genetic component.
- What are the symptoms of COPD?Symptoms may include shortness of breath, with or without cough and mucus production. Over time, however, you typically will develop a cough, particularly when exerting yourself, such as when exercising or climbing the stairs. You may also notice that you’ve cut back on certain activities because they make you too tired or cause shortness of breath or chest tightness.
- How can I be sure to get the right diagnosis?Studies find that doctors are not very good at diagnosing COPD in women because it’s long been considered it a man’s disease. If you think you might have COPD, ask your health care professional to test your lung function with spirometry.
- Is there a cure for COPD?While there is no cure for COPD, early treatment can improve symptoms, help patients breathe better and reduce the risk of exacerbations, or sudden worsening of COPD.
- What medications are used to treat COPD?A variety of medications are used to treat COPD, including long- and short-acting bronchodilators, inhaled corticosteroids and a PDE-4 inhibitor. When exacerbations occur, systemic glucocorticoids or antibiotics might be used as well.
- How will I know what medication is best for me?You and your doctor will decide on the best medication for you based on your symptoms, the severity of your COPD, other medical conditions you have and your lifestyle.
- How will I know if I need surgery?Surgery is reserved for the sickest COPD patients whose symptoms can no longer be controlled by medications. You and doctor can determine if you are eligible for surgery.
- How can I prevent exacerbations?You may be able to prevent or reduce the frequency of exacerbations by following your doctor’s recommended treatment plan; taking your medication as prescribed; quitting smoking; getting vaccinated against the flu and pneumonia; and participating in pulmonary rehabilitation.



