What is Colon Cancer???
Overview
Colorectal cancer is one in every of the foremost common cancers within the us. About one in twenty individuals can develop cancer of the colon or body part in their lifetimes. It is also the second leading reason behind cancer deaths once men girls|and ladies|and girls} square measure thought-about along and is that the third leading reason behind cancer death among women.
There square measure regional variations in body part cancer’s incidence and mortality throughout the country, with the bottom rates occurring among those living in Western states, and survival rates lowest among African Americans.
The good news is that the illness isn’t solely extremely conquerable and treatable, however conjointly extremely preventable. Regular screening and removal of polyps will scale back body part cancer risk by up to ninety %. But sadly, fear, denial and embarrassment keep many folks from being screened.
When carcinoma is caught and treated in stage I, there’s a seventy four % probability of survival at 5 years. Once the cancer is larger and has spread to the lymph nodes, however, the five-year survival rate drops to 46 percent. If the cancer has already spread to distant parts of the body such as the liver or lungs, the five-year survival rate goes down to 6 percent.
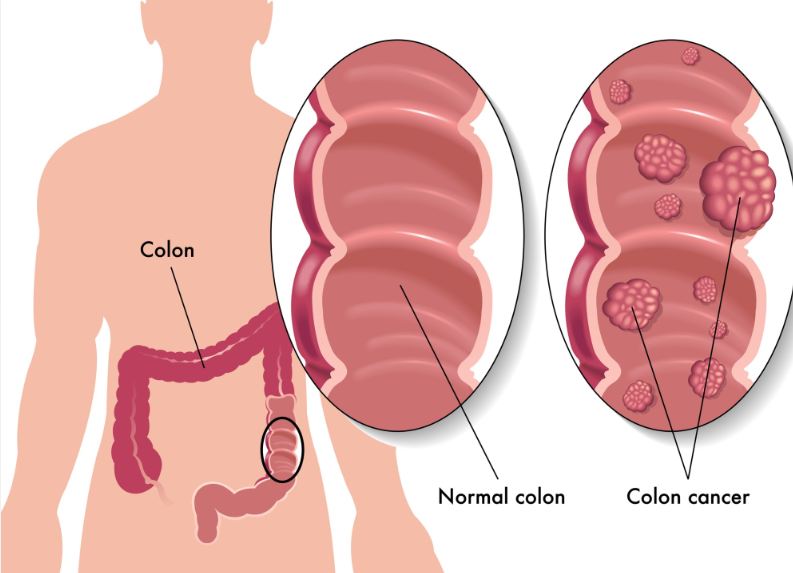
The large gut is that the last section of the epithelial duct and consists of the colon and body part. The colon is four to 6 feet long, and the last seven to nine inches of it is called the rectum. After food is digested in the stomach and nutrients are absorbed in the small intestine, waste from this process moves into the colon, where it solidifies and remains for one or two days until it passes out of the body.
Sometimes the body produces an excessive amount of tissue, ultimately forming a neoplasm. These tumors can be benign (not cancerous) or malignant (cancerous). In the large intestine, these tumors are called polyps. Polyps are found in about 30 percent to 50 percent of adults. People with polyps in their colon tend to continue producing new polyps even after existing polyps are removed.
There are several types of polyps, the most common being hyperplastic polyps, adenomatous polyps, sessile serrated polyps and malignant polyps. Hyperplastic polyps are typically not precancerous. Adenomatous polyps (also called “adenomas”) and sessile serrated polyps may undergo cancerous changes, becoming adenocarcinomas. Malignant polyps are already cancerous.
Colon cancers develop from precancerous polyps that grow larger and eventually transform into cancer. It is believed to require concerning ten years for alittle metastatic tumor polyp to grow into cancer. Therefore, if acceptable body part cancer screening is performed, most of those polyps is removed before they turn out to be cancer, effectively preventing the development of colon cancer.
Besides adenocarcinomas, there are other rare types of cancers of the large intestine, including carcinoid tumors typically found in the appendix and rectum; gastrointestinalstromal tumors found in the connective tissue of the colonic or body part wall; and lymphomas, that square measure malignancies of immune cells that may involve the colon, rectum and lymph nodes.
Risk Factors
The exact reason behind carcinoma is unknown, however it seems to be influenced each by hereditary and environmental factors. People at Associate in Nursing redoubled risk of carcinoma embody those with either a private or case history of body part cancer or polyps, people with a long-standing history of inflammatory bowel illness and other people with familial body part cancer syndromes. Some of those at high risk could have a 100% probability of developing body part cancer.
Specific risk factors include:
- Personal History: A private history of body part cancer, benign colorectal polyps which are adenomas or sessile serrated polyps, or chronic inflammatory bowel disease (e.g., ulcerative colitis and Crohn’s disease) puts you at increased risk for colorectal cancer. In fact, those who have had body part cancer square measure a lot of possible to develop new cancers in alternative areas of the colon and body part, despite previous removal of cancer.
- Heredity: If one in every of your folks, siblings or children has had colorectal cancer or a benign adenoma, you have a higher risk of developing colorectal cancer. If 2 or a lot of shut relatives have had the illness, you also have an increased risk; approximately 20 percent of all people with colorectal cancer fall into this category. Your risk is even greater if your relatives were affected before age 60 or if more than one close relative is affected.Additionally, there are two genetic conditions—familial adenomatous polyposis (FAP) and hereditary nonpolyposis colorectal cancer (HNPCC)—that lead to colorectal cancer in about 5 percent of patients.
- Familial adenomatous polyposis (FAP). People who have transmissible the FAP syndrome could develop a whole lot to thousands of polyps in their colon and body part at a young age, usually in their teens or early adulthood. These polyps are all adenomas. By age 40, most patients with FAP can develop carcinoma if they do not have preventive surgery. Most people United Nations agency have this syndrome begin annual colon examinations whereas in primary school, and many choose to have their colon and rectum removed before cancer develops. FAP is rare, accounting for about 1 percent of all cases of colorectal cancer.
- Hereditary non-polyposis colon cancer (HNPCC). Also referred to as kill Syndrome, HNPCC is a more common form of inherited colon cancer, accounting for about 3 percent to 5 percent of all colorectal cancer cases. While it’s not related to thousands of polyps, polyps are present and grow more quickly into cancer than in patients without HNPCC. Colon cancer in individuals with HNPCC conjointly develops at a younger age than periodic carcinoma, although not as young as in those with FAP.Cancers in patients with HNPCC tend to be quick growing and respond less to therapy. The period risk of carcinoma in individuals with HNPCC could also be as high as eighty %. People with HNPCC are also at an increased risk for other types of cancer, including cancer of the ovary, uterus, stomach, kidney andbladder.
- MUTYH-associated polyposis (MAP): People with this syndrome, which is caused by mutations in the gene MUTYH, develop colon polyps that are destined to become cancerous if they are not removed. Their colonoscopyfindings may be similar to FAP with hundreds to thousands of polyps or not. People with MUTYH are also at increased risk of cancers of the small intestine, skin, ovary and bladder.
There are some additional rare genetic mutations associated with colon cancer. These include Turcot syndrome, an inherited condition in which people are at an increased risk of adenomatous polyps (and thus, colon cancer) and brain tumors, and Peutz-Jeghers syndrome, a condition that leads to freckles around the mouth and sometimes on the hands and feet, as well as large polyps in the digestive tract and an increased risk of colon and other cancers at a young age.
In addition, there are several gene mutations found in Jews of Eastern European descent (Ashkenazi Jews) that increase colon cancer risk. The most common mutation, which is called the I1307K APC mutation, is found in 6 percent of American Jews.
If you have a history of adenomas or colon cancer or suspect you have a family history of the disease, you should discuss this with your health care professional because you may need to begin screening for the disease at a relatively young age. In some cases, you may wish to undergo genetic testing.
- Age: The risk of colorectal cancer increases with age. Ninety percent of new cases of colorectal cancer in the United States are in people over 50. Clinical studies indicate that when screened for the disease, African Americans tend to be diagnosed with colorectal cancer at a younger age than Caucasians.
- Race: African Americans are more likely to get colorectal cancer than any other ethnic group. Compared to Caucasians, African Americans are about 10 percent more likely to develop colorectal cancer. Unfortunately, they also are more likely to be diagnosed in advanced stages. As a result, African Americans are more likely to die from colon cancer than Caucasians. In 2007, the rate of death from colon cancer among African Americans was 44 percent greater than that among whites.
- Diet: Eating a diet high in processed meats (hot dogs and some lunch meats) and red meats (lamb, beef or liver) may increase your risk of developing the disease. Avoiding red meat and eating a low-fat diet rich in vegetables, fruit and fiber (e.g., broccoli, whole grains and beans) may reduce your risk of developing colorectal cancer. Some studies suggest that boosting calcium intake helps prevent colon cancer. Until further studies are done, men should keep their intake below 1,500 milligrams because of the increased risk of prostate cancer associated with high levels of calcium. Some research has also shown that vitamin D, which you can get from foods, sun exposure or a pill, can help lower colon cancer risk, but because of the increased risk of skin cancer with sun exposure, most health care professionals don’t advocate getting more sun to reduce colorectal cancer at this time. Other studies suggest that taking a multivitamin that contains folic acid may lower colon cancer risk, but more study is needed in this area. There is some research suggesting that a diet high in magnesium may decrease colon cancer risk, especially in women. More research is necessary to find out if this link exists.
- Lifestyle: Regular exercise is a key weapon in the fight against colorectal cancer. Another significant risk factor in colorectal cancer is smoking. Get help quitting if you can’t do it on your own. And keep your alcohol intake to one drink a day or less (two drinks a day or less for men).
- Obesity: Obesity is an epidemic in the United States and has been associated with many types of cancers, including colorectal cancer. There is a strong link between higher BMI (body mass index) and waist circumference and colon cancer risk in men and a weaker association seen in women. High levels of insulin and insulin-like growth factor may play a role in development of colon cancer in obese people. Weight loss has been shown to reduce the risk of colon cancer.
Screening Tests
The American Cancer Society recommends all women and men over the age of 50 who are at average risk of colorectal cancer undergo one of the following:
- A fecal occult blood test once a year. This test detects microscopic amounts of blood in the stool and only detects tumors that are bleeding. This must be performed on three separate bowel movements, and you should avoid nonsteroidal anti-inflammatory medications (NSAIDS) for seven days and vitamin C and red meat for three days before collecting the stool samples. Your health care skilled provides the mandatory materials to gather the stool specimens for straightforward testing reception or within the workplace. The stool ought to be collected before it’s within the essence. A wooden stick is used to smear a small sample of stool onto the slots in the test card. You will get 3 take a look at cards, which, when completed, you return to your health care professional. Your health care skilled could advocate this take a look at prior age fifty or a lot of oftentimes if you’re at high risk for carcinoma and/or polyps.
- A flexible sigmoidoscopy five years. This examination allows the health care professional to inspect the rectum and lining of the left colon with a thin tube with a light and camera on the end. To prepare for the test, you may be asked to follow a special diet (such as drinking only clear liquids) for a day before the exam and to use enemas or laxatives to clean out your colon. The flexible sigmoidoscope is inserted into the body part whereas you lie on your left aspect. Sedative medication is not usually given for this procedure. This test is both diagnostic and therapeutic. However, it can only detect polyps or cancer accurately in the last two feet of the large intestine. Unfortunately, the sigmoidoscopy visualizes less than half the colon and misses about half of cancers and polyps that are close to becoming cancer in the first two to three feet of the colon.
- Fecal Immunochemical Test (FIT) every year. Similar to FOBT, FIT is a stool test that also detects hidden blood (occult) in the stool and must be performed every year. However, it tests for hidden blood in a different way than FOBT and has fewerfalse positive results. Some forms of FIT only require two stool specimens versus three for the FOBT, and neither vitamins nor foods will affect FIT results (these things can affect results of a FOBT); therefore, no dietary restrictions are necessary prior to collecting the stool samples. You perform the test in a similar manner as the FOBT. Similar to FOBT, the FIT test will not detect a tumor that is not bleeding, so a colonoscopy may be necessary for further screening or if cancer is suspected.
- Stool DNA at an uncertain frequency (manufacturer recommends every five years). A new screening approach, this test is available but not yet certified by the FDA. This test detects abnormal DNA shed by tumor cells into the stool and requires an entire stool sample. Studies are under way to determine how often the test should be done and how to increase its accuracy.
- A double contrast barium enema every five years. This take a look at involves injecting metallic element (a liquid imaging agent that shows up throughout associate X-ray) through the body part into the colon, then taking X-rays of the colon. A health care professional injects the thick, chalky liquid through a small tube inserted into your anus. You may feel an urge to move your bowels, but should hold on while the X-rays are taken. After the X-rays finish, you can expel the liquid. To avoid becoming constipated afterward, you should drink plenty of fluids to flush the barium from your system. While the procedure are often uncomfortable, it is not usually painful. This test is only a diagnostic test. If abnormalities show up, a colonoscopy must be performed. The enema isn’t a really sensitive take a look at and misses half polyps that area unit larger than one centimetre.
- A colonoscopy every 10 years. Similar to the flexible sigmoidoscope, the colonoscope is a longer thin black tube that allows the health care professional to examine the entire large intestine. Preparation for the procedure requires drinking alaxative the day before the colonoscopy. Adequate preparation is critically vital to change the medico to see the whole lining of the colon. Leftover stool obscures the view of that portion of the colon and could lead to missing lesions. The ACS recommends obtaining a endoscopy beginning at age fifty for the average-risk person or if a FOBT or work shows blood within the stool. You typically receive a gentle sedative throughout the procedure, so you should experience minimal discomfort. The procedure itself typically lasts 20 to 30 minutes.This test is both diagnostic and therapeutic. It detects polyps and cancers found anywhere in the colon. Any polyps or different growths found throughout this examination area unit typically removed and sent to a laboratory for examination. Medicare currently covers this procedure each ten years for individuals over fifty WHO area unit thought-about average risk for developing carcinoma and each 2 years for individuals at high risk. Women and men over fifty ought to have a endoscopy a minimum of each ten years. The yank faculty of medicine recommends that African Americans, who tend to develop the disease at a younger age than other races, begin getting screening colonoscopies at age 45.
- CT colonography (virtual colonoscopy) every five years. This is a relatively new technique that uses a CT scan to create a three-dimensional image to evaluate the colon. It doesn’t yield a diagnostic assay (tissue sampling) or polyp removal if any abnormalities area unit found. You must take a laxative the day before this test, similar to a colonoscopy, and if any abnormalities are found, you must undergo a colonoscopy. Most insurance firms don’t cowl virtual colonography as screening for large intestine cancer.
Most women find sigmoidoscopies and colonoscopies much more tolerable than they expect. Worrying about the process and undergoing the necessary preparation beforehand are often more unpleasant than the exam itself. Of the above-mentioned tests, colonoscopy is the preferred screening/prevention test, and FIT is the preferred test for patients who decline invasive cancer prevention tests.
Other tests that your health care provider might perform include:
- Digital rectal examination (DRE). Your health care professional inserts a gloved finger into the rectum to feel for any abnormalities. This simple test, which may be uncomfortable but usually is not painful, can detect many rectal cancers. However, even the longest of fingers are far too short to examine the full length of the large intestine. For this reason, other tests and examinations, such as the FOBT, flexible sigmoidoscopy and colonoscopy must be used. The rectal exam is not sufficient to screen for colon cancer.
- Genetic testing. The few hereditary cancer syndromes mentioned here are rare but are associated with mutations in specific genes. These mutations can be passed on to other family members. Thus, if your family is affected or may be affected by one of these syndromes, you may need to undergo genetic testing. If genetic testing and counseling are done properly, lives can be changed dramatically, both in terms of preventing colon cancer and lessening the psychological impact of knowing you are predisposed to the disease.Genetic testing for colon cancer raises many scientific and ethical issues. Although tests are available to identify the mutations that may predispose you to colon cancer, they are not absolutely positive predictors. Additionally, some health care professionals are not yet fully educated about the tests and may misinterpret the results.Thus, if you have a strong family history of colon cancer, you should be seen at agenetic screening center. Talk to your health care professional about the genetic screening process and how to locate such a center.
If there is a reason to suspect that you have colorectal cancer, your health care professional will take a complete medical history and perform a physical examination as part of an initial evaluation.
Symptoms
Symptoms of colorectal cancer include:
- Change in bowel habits (diarrhea, constipation or narrow stools for more than a few days)
- Urgency for a bowel movement or feeling like you need to move your bowels even if you just did
- Blood in the stool
- Stomach pain
- Weakness and/or fatigue
Contact your health care professional if you experience one or more of these symptoms.
Diagnosis
Because the symptoms of carcinoma square measure imprecise and generally occur late within the development of the cancer, a spread of tests square measure accustomed each screen and diagnose the illness. Screening tests search for illness in people who look and feel healthy, ideally catching the illness as early as potential or, within the case of carcinoma, even before the precancerous lesion has turned into cancer. Diagnostic tests search for the cause and verify the extent of the illness in somebody United Nations agency has obvious symptoms.
A viscus preparation is commonly needed before several of those tests, particularly a endoscopy. This involves cleaning out your bowel the night before the test with a laxative solution. It is important that the bowel be clean so the physician performing the colonoscopy gets the best look at your colon. Since some preparations will have an effect on your blood level certainly electrolytes, your health care skilled can tell you which ones preparation to use for your procedure.
Diagnostic Tests
- Flexible sigmoidoscopy or colonoscopy. Sigmoidoscopy may be a procedure that permits a Dr. to look at the liner of the body part and also the lower a part of the colon. This space accounts for fewer than common fraction the whole space of the body part and colon. If a mass or any other types of abnormalities are seen through the flexible sigmoidoscope or colonoscope, a sample (biopsy) is taken for further examination by a pathologist to determine if it is cancerous or benign.
- Complete blood count (CBC) and blood chemistry. The CBC determines whether you are anemic because many people with colorectal cancer become anemic due to prolonged bleeding from the tumor.
- Computed tomography (CT). In this test, a rotating X-ray beam creates a series of pictures of the body from many angles, helping visualize any masses that may indicate that the colon cancer has spread to your liver or other organs.
- Magnetic resonance imaging (MRI): Like CT, magnetic resonance imaging displays a cross-section of the body. However, MRI uses powerful magnetic fields and radio waves instead of radiation.
- Chest x-ray. This familiar imaging test detects if colorectal cancer has spread to the lungs.
- PET scanning: This check will verify if sure cells square measure victimisation aldohexose quite different cells. Cancer cells, that square measure actively dividing, use more glucose so they light up on a PET scan. This test is used to follow cancer and can be combined with a CT scan to better localize a possible recurrence. It is important to remember that not all tumors will be responsive to PET/CT imaging.
Colorectal Cancer Stages
As with all cancers, there are various stages of colon cancer:
- Stage 0: Abnormal (dysplastic) cells have been found in the innermost lining (mucosa) of the colon. This stage is also known as carcinoma in situ or intramucosal carcinoma, and there is a very small chance these cells have spread, so this stage is not considered to be invasive cancer.
- Stage I: Cancer has spread to the inside lining of the colon but hasn’t spread beyond the colon wall or rectum.
- Stage II: Cancer has spread through the colon or rectum and may invade surrounding tissue, but no lymph nodes are involved.
- Stage III: Cancer has spread to the lymph nodes, but not to distant sites.
- Stage IV: Cancer has spread to other distant parts of the body, such as the liver or the lung.
Treatment
Surgery is often required to treat colorectal cancer. The surgical procedure used depends on where the cancer is located. Most patients United Nations agency endure surgery for carcinoma have AN open abdominal operation, wherever the operating surgeon makes AN incision within the abdomen and removes the growth and any affected body fluid nodes. In some cases, however, a procedure called laparoscopic colon cancer resection may be used. Like open abdominal surgery, laparoscopic surgery is performed under general anesthesia, but multiple, much smaller incisions are made, which leads to a shorter recovery time. Studies have shown similar results once open abdominal and laparoscopic techniques square measure accustomed take away carcinoma. A operating surgeon veteran at laparoscopic surgery ought to perform these surgeries.
Occasionally, early cancerous changes may be limited to a portion of an otherwise noncancerous polyp. In these cases, it is sometimes possible to remove some very early colon cancers during a colonoscopy.
If a part of the colon must be removed thanks to a bigger cancerous growth, the surgeon will remove the affected portion and leave as much of the healthy colon behind as possible. In rectal cancer, the rectum is removed.
In several cases, the surgeon will be able to reconnect the healthy portions of the colon and rectum, which allows waste to flow through the colon to the rectum. If this is not possible, you may need to have a colostomy. A ostomy (stoma) involves making a hole within the wall of abdomen to that AN finish of your colon is hooked up thus you’ll eliminate waste into a special bag. Depending on the situation, a colostomy may be temporary or permanent.
You may be stated AN enterostomal healer (a health care skilled, often a nurse, trained to help people with their colostomies) as part of your initial workup. The enterostomal healer will address issues concerning however a ostomy may have an effect on your daily activities.
Even after colon cancer has been completely removed with surgery, cancer cells can remain in the body and cause relapse. To kill these cells and decrease the chances of a relapse, health care professionals use chemotherapy. Not all people need chemotherapy after surgery. Those presumably to receive therapy square measure individuals in danger for return, namely, those with stage III colon cancer or high risk stage II.
For some rectal cancers, chemotherapy is given along with radiation therapy in an attempt to shrink the tumor before surgery. This is called neoadjuvant chemotherapy.
Several chemotherapy drugs are used to treat colon cancer. In many cases, two or more of these drugs are combined for more effective treatment:
- 5-Fluorouracil (5-FU): 5-FU is part of most chemotherapy treatments for colorectal cancer, and it is often given together with another chemotherapy drug called leucovorin (folinic acid). 5-FU may be given through a vein over two hours or as a quick injection followed by continuous infusion via a battery-operated pump over the following one or two days. In most cases, patients get 5-FU every two weeks for six months to a year. Side effects include nausea, loss of appetite, diarrhea, low blood cell counts and sensitivity to sunlight.
- Capecitabine (Xeloda): A chemotherapy drug in pill form, Xeloda changes to 5-FU once it reaches the tumor and is about as effective as continuous intravenous 5-FU. Patients taking capecitabine usually get it twice a day for two weeks, followed by a week off. Capecitabine is a convenient option to 5-FU because it can be taken at home, but it still has similar side effects.
- Irinotecan (Camptosar): This drug is often combined with 5-FU and leucovorin in a regimen called FOLFIRI. Irinotecan may also be used by itself as a second-line therapy if other chemotherapy drugs are not effective. It is given intravenously over 30 minutes to two hours. Some people cannot break down irinotecan, which leads to severe side effects like diarrhea and low blood counts. This inability to break down the drug is due to an inherited gene variation that can be tested for, so it is possible to predict how you will react. If you are taking irinotecan and experience severe side effects, call your doctor right away.
- Oxaliplatin (Eloxatin): For the treatment of advanced large intestine cancer, oxaliplatin is usually given together with 5-FU and leucovorin (known as the FOLFOX regimen) or with capecitabine (known as the CapeOX regimen) as a first- or second-line treatment. It may also be used as adjuvant therapy after surgery for colorectal cancers at earlier stages. Patients take oxaliplatin intravenously over two hours, usually once every two or three weeks. Oxaliplatin may affect peripheral nerves, leading to numbness, tingling and heightened sensitivity to temperature, especially in the hands and feet. In most cases, these side effects go away once patients stop taking the medication, but they can persist. Talk to your doctor about potential side effects before you start taking oxaliplatin.
Individuals with advanced carcinoma could receive targeted medication that facilitate stop cancerous tumors from growing. These drugs include bevacizumab (Avastin), cetuximab (Erbitux) and panitumumab (Vectibix). They may incline alone or along side therapy.
Not all people benefit from targeted medications. Researchers are currently examining who are most likely to respond. Until then, health care professionals will continue to weigh the risks and benefits of targeted drugs before they prescribe them for people with advanced disease.
Radiation therapy could profit some individuals with body part cancer, but it is not usually used in the treatment of early stage colon cancer. Like therapy, radiation is also useful for patients UN agency ar at high risk of cancer return, for example if the cancer has unfold to near organs. In general, the goal of radiation is to scale back possibilities of carcinoma return instead of to enhance survival.
For those whose colorectal cancer has metastasized to a few areas in the liver, lungs or elsewhere in the abdomen, surgically removing or destroying these metastases can increase survival.
If the cancer comes back in only one part of the body, you may need surgery again. If it has spread to several parts of the body, you may receive chemotherapy and/or radiation therapy.
Prevention
The most vital line of defense against large intestine cancer is screening for large intestine cancer. You should follow the established pointers for screening procedures so any malignant neoplasm polyps is removed before they transform cancer and, if cancer exists, it can be detected at the earliest possible stage. If you’re at average risk of large intestine cancer, the yank Cancer Society recommends that every one ladies and men over the age of fifty endure one among the following:
- annual fecal occult blood test
- flexible sigmoidoscopy every five years
- double contrast barium enema every five years
- colonoscopy every 10 years unless you are African American, in which case your screening can begin at age 45
- virtual colonoscopy (CT colonography) every five years
- stool DNA testing, interval uncertain (a new screening approach, this test is available but not yet certified by the FDA)
Any positive screening test should be followed by an appropriate and complete diagnostic evaluation of the colon including a colonoscopy with biopsies, if necessary.
If you are at an increased risk of colorectal cancer or adenomas because of a family history of cancer or polyps, you should follow the above recommendations and also:
- Begin colorectal screening at age 40, or 10 years before the youngest case of colon cancer in the immediate family.
- Discuss genetic counseling and/or testing with your health care professional.
If you’re at associate redoubled risk for large intestine cancer for a reason apart from case history, such as a personal history of inflammatory bowel disease, you may also need to begin screening before age 50. Screening recommendations vary supported your specific risk factors; discuss your individual screening schedule together with your health care skilled.
Modifying your diet and exercise could facilitate decrease your risk of forming colon polyps and/or carcinoma. A diet made in vegetables, fruit and fiber and low in fat may reduce the risk of developing colon cancer. Some counsel that increasing intakes of Ca and cholecarciferol will facilitate stop carcinoma. (Men ought to keep their intake below one,500 milligrams because of the increased risk of prostate cancer associated with high levels of calcium.) Calcium can be found in dairy products, calcium-fortified products such as orange juice, soy and dark green vegetables. Other research has shown that taking a multivitamin containing folic acid (a B complex vitamin) decreases the risk of colon cancer, but more study is needed. There is some analysis suggesting that a diet high in metallic element could decrease carcinoma risk, especially in women. More research is necessary to find out if this link exists.
Regular exercise is important in preventing colon cancer. Experts say that vigorous exercise is not necessary. Instead, just incorporate more activity into your daily routine, such as taking the steps instead of the elevator or parking your car farther from the building you are entering. Overall, the yank Cancer Society recommends half-hour of physical activity a minimum of 5 days per week and says that forty five minutes or a lot of of moderate to vigorous activity five or a lot of days every week could additional scale back the chance of colon, breast, uterine and prostate cancers.
It is conjointly well to drink alcohol solely moderately (no over one street drug per day for girls, for a total of less than seven drinks per week, and no over 2 alcoholic beverages for men, for a total of less than 14 drinks per week) and abstain from tobacco use.
Results from multiple studies show that individuals UN agency often take Bayer and different non-steroidal medicinal drug medications (NSAIDS) have a lower risk of large intestine cancer and adenomatous polyps. An August 2009 study printed within the Journal of the yank Medical Association found that Bayer will facilitate stop large intestine cancer deaths in addition. The study looked at 1,279 men and women with colon cancer and found that those who took aspirin regularly after their diagnoses were 30 percent less likely to die from the disease than people who didn’t take aspirin. However, the risk of stomach ulcers and other side effects associated with aspirin and NSAIDS may outweigh the benefits. Therefore, specialists don’t suggest individuals at average risk of large intestine cancer take NSAIDS as a interference strategy. Discuss the potential risks and benefits of taking NSAIDS with your health care professional.
Facts to Know
- The American Cancer Society estimates that about 103,170 new cases of colon cancer and 40,290 new cases of rectal cancer will be diagnosed in 2012. Combined, these cancers are predicted to cause about 51,690 deaths during 2012.
- While colorectal cancer is the second leading cause of cancer deaths when men and women are considered together and is the third leading cause of cancer death among women, incidence among Caucasians in the United States has been decreasing, perhaps due to improved screening methods. Among African Americans, however, incidence rates have remained relatively stable.
- The risk of developing colorectal cancer is highest among those with a family history of colorectal cancer or adenomatous polyps and those who have inflammatory bowel disease.
- Except for those with hereditary conditions that may predispose them to developing colorectal cancer relatively early in life, 90 percent of all cases occur after the age of 50.
- Tumors that grow in the large intestine are called polyps. A biopsy determines if the polyp is benign (not cancerous) or malignant. Benign polyps can be precancerous (adenomatous and sessile serrated) or not precancerous (hyperplastic). Thirty percent to 50 percent of the population has polyps. Over the course of about 10 years, adenomatous polyps can become cancerous if they are not removed.
- Undergoing appropriate screening for colorectal cancer can decrease death rates from this cancer by up to 90 percent. Colorectal cancer screening is designed to detect and remove precancerous polyps (adenomas and sessile serrated polyps) before they turn into cancer and to diagnose cancer at the earliest stages.
- If you or a close relative were diagnosed with colon cancer at age 45, then other members of your family should begin screening around age 35. If you have a close relative with colorectal cancer, you should begin screening at the age of 40 or 10 years before the age at which the youngest relative was diagnosed with cancer.
- Cancer specialists are using more aggressive strategies to make sure cancer does not return after surgery. You may receive both chemotherapy and radiation therapy to increase your chances of a complete cure. These treatments destroy microscopic accumulations of cancer cells that cannot be seen or removed during surgery.
- When colon cancer is caught and treated in stage I, there is a 74 percent chance of survival at five years. Once the cancer is larger and has spread to lymph nodes, the five-year survival rate drops to 46 percent. If the cancer has already spread to distant parts of the body such as the liver or lungs, the five-year survival rate goes down to 6 percent.
- You may be able to reduce your risk for colorectal cancer by eating a diet high in fiber and low in fat, getting plenty of exercise, limiting your alcohol intake to one drink or less a day, losing weight if you are obese, taking calcium and having regular colorectal cancer screenings.
Key Q&A
- My health care professional told me I have polyps. What are these and how will they be treated?Colorectal polyps are excess growths of tissue in the lining of your colon or rectum. They can be noncancerous (hyperplastic), precancerous (adenomas or sessile serrated polyps) or malignant (cancerous). All colorectal cancers develop from precancerous polyps. Therefore, if these precancerous polyps are removed during colonoscopy or sigmoidoscopy, they will no longer be able to grow into cancer. Most colorectal polyps are easily removed during colonoscopy without the need for surgery. Once you have polyps, you are at increased risk for developing more polyps in the future and need repeated screening to detect and remove them.
- My father and grandmother both had colon cancer. What are my risks and what should I do?First, realize the disease is highly curable when diagnosed early. When the cancer spreads to other distant places like the lung or liver, however, the survival rate is less than 10 percent. A family history of colon cancer or adenomatous polyps significantly increases your chances of developing the disease, and the more family members you have with colon cancer, the higher your risk. Make an appointment with your health care professional now to discuss your personal and family health history and to determine the next steps you should take. You will need to have colorectal cancer screening starting at the age of 40 or 10 years before the age at which the youngest relative was diagnosed with cancer. You will probably have regular surveillance of your colon by colonoscopy.
- Is there any way to reduce my risks for colon cancer?Most important is to ask your health care professional about colorectal cancer screening beginning at age 50 (45 for African Americans) if you are at average risk or earlier if you have family members (such as your father, mother, sister or brother) who had colorectal polyps or cancer. If you undergo appropriate screening for colorectal cancer, you may decrease your risk of death from colorectal cancer by 90 percent. This is because physicians can detect and remove precancerous polyps before they turn into cancer, most effectively by colonoscopy. Research increasingly suggests that a diet high in fiber, fruits and vegetables and low in fat may help reduce your risk for colon cancer. Losing weight if you are obese may decrease your risk of colorectal cancer. Taking calcium and vitamin D may prevent formation of precancerous polyps and colon cancer. And getting regular exercise may help, too.
- My health care professional told me my cancer had metastasized and that I had a “met” in another place besides the colon. What does that mean?“Met” is short for metastasis, which means the cancer has spread to other parts of the body. Any time your health care professional uses a word you don’t understand, stop him or her right there and ask what that word means.
- What are my chances of a cure?No one really knows if cancer is totally cured. But it is sometimes pushed back so far it never grows again, which is called achieving remission or long-term survival. Your chances of surviving for a long time largely depend on the stage of your cancer at the time of diagnosis and the success of treatments you receive. The earlier the cancer is detected, the higher your chances for long-term survival.
- My cancer is pretty advanced. How long have I got?Any number that a health care professional gives you is based on estimates derived from experiences with other patients. No one can tell you what your specific chances are. Survival averages are just that: averages.
- What can I do about this ongoing pain?One of the worst things that cancer patients do is to suffer pain when they do not have to! Discuss your pain with your health care professional so that you can get the relief you need. It might be necessary to see a pain specialist. Most health care professionals can refer you to someone who specifically handles chronic pain problems. If you have severe pain, narcotics may be the best type of medicine.
- What caused this? Was it something I did? How long did it take to grow?No one is really sure what causes colorectal cancer. It’s very unlikely that it was something you did. The tendency to get the disease may be hereditary, that is, it may run in families. A polyp in your colon can take as many as 10 years to become cancerous. Colorectal cancer is difficult to find without regular screening and often does not cause symptoms until it’s already well developed. So don’t beat yourself up that you didn’t “catch” it a few months ago.



