What is Estrogen???
Overview
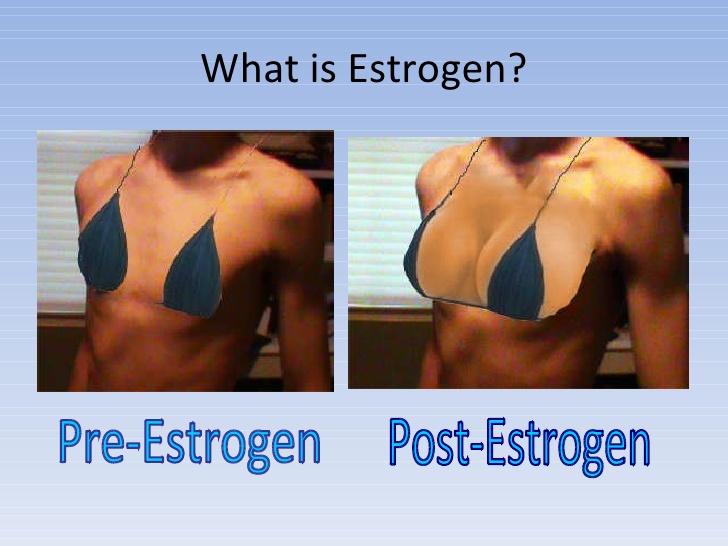
Estrogen is perhaps the foremost wide acknowledged and mentioned of all hormones. The term “estrogen” actually refers to any of a group of chemically similar hormones; estrogenic hormones are sometimes mistakenly referred to as exclusively female hormones when in fact both men and women produce them. However, the role steroid hormone plays in men isn’t entirely clear.
To understand the roles estrogens play in ladies, it’s vital to know one thing regarding hormones normally. Hormones square measure very important chemical substances in humans and animals. Often brought up as “chemical messengers,” hormones carry data and directions from one cluster of cells to a different. In the frame, hormones influence virtually each cell, organ and performance. They regulate our growth, development, metabolism, tissue perform, sexual function, reproduction, the way our bodies use food, the reaction of our bodies to emergencies and even our moods.
The Role of Estrogen in Women
The steroid hormones square measure unambiguously to blame for the expansion and development of feminine sexual characteristics and replica in each humans and animals. The term “estrogen” includes a gaggle of with chemicals similar hormones: estrogen, oestradiol (the most superabundant in ladies of fruitful age) and oestrogen. Overall, steroid hormone is made within the ovaries, adrenal glands and fat tissues. More specifically, the estradiol and estrone forms are produced primarily in the ovaries in premenopausal women, while estriol is produced by the placenta during pregnancy.
In women, steroid hormone circulates within the blood and binds to steroid hormone receptors on cells in targeted tissues, poignant not solely the breasts and female internal reproductive organ, but also the brain, bone, liver, heart and other tissues.
Estrogen controls growth of the female internal reproductive organ lining throughout the primary a part of the oscillation, causes changes in the breasts during adolescence and pregnancy and regulates various other metabolic processes, including bone growth and cholesterollevels.
Estrogen & Pregnancy
During the fruitful years, the hypophysis within the brain generates hormones that cause a brand new egg to be discharged from its vesicle monthly. As the follicle develops, it produces estrogen, which causes the lining of the uterus to thicken.
Progesterone production will increase when biological process within the middle of a woman’s cycle to organize the liner to receive and nourish a animal thus it will turn out to be a foetus. If fertilization doesn’t occur, estrogen and progesterone levels drop sharply, the lining of the uterus breaks down and menstruation occurs.
If fertilization will occur, steroid hormone and progestin work along to forestall extra biological process throughout physiological condition. Birth control pills (oral contraceptives) take advantage of this effect by regulating hormone levels. They conjointly lead to the assembly of a really skinny female internal reproductive organ lining, called the endometrium, which is unreceptive to a fertilized egg. Plus, they thicken the cervical mucous secretion to forestall gamete from getting into the cervix associate degreed fertilizing an egg.
Oral contraceptives containing estrogen may also relieve menstrual cramps and some perimenopausal symptoms and regulate menstrual cycles in women with polycystic ovarian syndrome (PCOS). Furthermore, research indicates that birth control pills may reduce the risk of ovarian, uterine and colorectal cancer.
Other Roles of Estrogen
Bone
Estrogen made by the ovaries helps stop bone loss and works along with atomic number 20, vitamin D and other hormones and minerals to build bones. Osteoporosisoccurs once bones become too weak and brittle to support traditional activities.
Your body constantly builds and remodels bone through a process called resorptionand deposition. Up until around age 30, your body makes more new bone than it breaks down. But once estrogen levels start to decline, this process slows.
Thus, when climacteric your body breaks down additional bone than it rebuilds. In the years right away when climacteric, ladies could lose the maximum amount as twenty p.c of their bone mass. Although the speed of bone loss eventually levels off when climacteric, keeping bone structures sturdy and healthy to forestall pathology becomes additional of a challenge.
Vagina and Urinary Tract
When estrogen levels are low, as in menopause, the vagina can become drier and the vaginal walls thinner, making sex painful.
Additionally, the liner of the epithelial duct, the tube that brings body waste from the bladder to the skin of the body, thins. A small variety of ladies could expertise a rise in tract infections (UTIs) which will be improved with the employment of channel steroid hormone medical aid.
Perimenopause: The Menopause Transition
Other physical and emotional changes are associated with fluctuating estrogen levels during the transition to menopause, called perimenopause. This phase typically lasts two to eight years. Estrogen levels could still fluctuate within the year when climacteric. Symptoms include:
- Hot flashes—a sharp sensation of warmth in your face, neck and chest that may cause you to sweat profusely, increase your pulse rate and make you feel dizzy or nauseous. A flush generally lasts regarding 3 to 6 minutes, although the sensation can last longer and may disrupt sleep when it occurs at night.
- Irregular menstrual cycles
- Breast tenderness
- Exacerbation of migraines
- Mood swings
Estrogen Therapy
Estrogen therapy is used to treat certain conditions, such as delayed onset of pubertyand menopausal symptoms such as hot flashes and symptomatic vaginal atrophy. Vaginal atrophy could be a condition during which low steroid hormone levels cause a woman’s channel to slim, lose flexibility and take longer to lubricate. Female incompetence, a condition in which the ovaries produce little or no hormones, as well as premature ovarian failure, can also cause vaginal dryness, breast atrophy and lower sex drive and is also treated with estrogen.
For many years, estrogen therapy and estrogen-progestin therapy were prescribed to treat menopausal symptoms, to prevent osteoporosis and to improve women’s overall health. However, when publication of results from the Women’s Health Initiative (WHI) in 2002 and March 2004, the U.S. Food and Drug Administration (FDA) now advises health care professionals to prescribe menopausal hormone therapies at the lowest possible dose and for the shortest possible length of time to achieve treatment goals. Treatment is mostly reserved for management of biological time symptoms instead of interference of chronic sickness.
The WHI was a study of 27,347 women aged 50 to 79 (mean age, 63) taking estrogen therapy or estrogen/progestin therapy. They were followed for a median of 5 and a 0.5 to seven years. The study was unable to document that benefits outweighed risks when hormone therapy was used as preventive therapy, and it found that risk due to hormones may differ depending on a woman”s age or years since menopause.
The National Cancer Institute found a really important drop by the speed of hormone-dependent breast cancers among ladies, the foremost common carcinoma, in 2003. In a study printed within the New England Journal of medication in April 2007, researchers speculated that the drop was directly associated with the actual fact that several ladies stopped taking internal secretion medical care in 2002 when the results of a significant government study found the treatment slightly enhanced a woman’s risk for carcinoma, heart disease and stroke. The researchers found that the decrease in breast cancer began in mid-2002 and leveled off after 2003. The decrease occurred in ladies over fifty and was marked in ladies with tumors that were oestrogen receptor (ER) positive—cancers that need oestrogen to grow. The researchers speculate that stopping the treatment prevented terribly little ER positive cancers from growing (and in some cases, possibly helped them to regress) because they didn’t have the additional estrogen required to fuel their growth.
However, for symptomatic biological time ladies or for ladies with premature climacteric, hormone therapy remains the most effective therapy for hot flashes. For more on the WHI study, guidelines for considering menopausal hormone therapy and its potential risks and benefits, visit the National Institutes of Health.
In addition to treating menopause-related symptoms, estrogen and other hormones are prescribed to treat reproductive health and endocrine disorders (the endocrine system is the system in the body that regulates hormone production and function).
Some uses of hormone therapy include the following situations:
- delayed puberty
- contraception
- irregular menstrual cycles
- symptomatic menopause
Diagnosis
Because internal secretion disorders will cause a good type of symptoms that are related to different conditions, a careful evaluation of your symptoms and general health is recommended, especially if you experience any unusual symptoms. To hit a designation, your health care skilled can wish to rule out bound conditions.
Your assessment will include a thorough personal medical history, a family medical history and a physical examination. Blood and different laboratory tests is also ordered to live internal secretion levels. Brain scans are sometimes ordered to identify abnormalities that may be affecting the endocrine system, and DNA testing can detect genetic abnormalities.
Estradiol or other hormone levels may be tested in the evaluation of precocious puberty in girls (the onset of signs of puberty before age seven), delayed puberty and in assisted reproductive technology (ART) to monitor ovarian follicle development in the days prior to in-vitro fertilization. Hormone levels also are generally wont to monitor HT.
Estrone and/or estradiol levels may be tested if you are having hot flashes, night sweats, insomnia and/or amenorrhea (the absence of periods for extended periods of time). However, due to the day-to-day and even hour-to-hour fluctuations in estradiol levels, they are less helpful than follicle stimulating hormone levels (FSH) for these evaluations. Salivary oestradiol testing is a smaller amount reliable still and of no price in designation or treating symptoms. In most cases, a woman’s age, symptoms and menstrual irregularity is sufficient for making the diagnosis.
Accurate diagnosis of hormonal disorders is important to determining appropriate treatment, which often includes estrogen therapy.
The following are common reasons estrogen therapy is prescribed:
- Delayed puberty. Delayed puberty can result from a variety of disruptions to normal hormone production, including central nervous system lesions, pituitary disorders, autoimmune processes involving the ovaries or other endocrine glands, metabolic and infectious diseases, anorexia or malnutrition, exposure to environmental toxins and over-intensive athletic training.Signs of delayed puberty include:
- Lack of breast tissue development by the age of 13
- No menstrual periods for five years following initial breast growth or by age 16
- Estrogen treatment for girls with delayed puberty is somewhat controversial; some health care professionals advise treatment, while others prefer close monitoring.
- Irregular menstrual periods. Once a medical analysis finds that there’s no different serious reason for your irregular cycles, oral contraceptives or cyclic progesterone may be used to regulate your cycle, assuming there is no reason you can’t use them. Polycystic ovarian syndrome is a common cause of irregular menstrual cycles.
- Contraception. Oral contraceptives containing estrogen are one of the most popular methods of fertility control in the United States. Other hormonal methods include some types of intrauterine devices (IUDs), the patch and an intravaginal ring.
- Menopausal Symptoms. Declining or unsteady levels of oestrogen and different hormones like androgen could begin as early because the late 30s. These secretion changes trigger several of the physical and emotional changes related to the transition to climacteric. Of course, climacteric may be a life stage, not a disease, but symptoms associated with menopause can be bothersome and concerning for some women.
These changes may include:
- Irregular menstrual periods
- Hot flashes (sudden warm feeling, sometimes with blushing or sweating)
- Night sweats (hot flashes that occur at night, often disrupting sleep)
- Fatigue (probably from disrupted sleep patterns)
- Mood swings
- Early morning awakening
- Vaginal dryness
- Fluctuations in sexual desire or response
- Difficulty sleeping
There is a wide range of possible menopause-related conditions. Ask your health care professional about any changes you notice.
For symptomatic menopausal women or women with premature menopause, HT or estrogen therapy (ET) remains the gold standard for relief of hot flashes and vaginally related symptoms. The estrogen-only medical care could solely be prescribed for ladies World Health Organization have had a excision and so aren’t in danger of female internal reproductive organ cancer. For perimenopausal ladies with these symptoms, oestrogen is typically given short-run (usually 2 to 5 years), with the goal of tapering and eventually discontinuing it.
If you’re experiencing moderate to severe biological time symptoms or not obtaining symptom relief from nonhormonal strategies, internal secretion medical aid is also Associate in Nursing possibility. (To find out about alternative, nondrug methods of relieving menopausal symptoms, visit the menopause topic at HealthyWomen.org.)
New, lower-dose versions of the internal secretion therapies accustomed treat symptoms of change of life area unit currently accessible. The U.S. Food and Drug Administration (FDA) has approved pills, skin patches, gels, lotions and sprays in lower doses. Delivery of sex hormone through the skin is also less possible than pills to cause blood clots within the legs or lungs.
The {estrogen|oestrogen|steroid internal secretion|steroid|sex hormone} dose used for hormone medical aid varies wide reckoning on the symptoms it’s supposed to manage, as does dosing schedule. Discuss your symptoms and concerns with your health care professional.
In 2003, the FDA declared that a replacement warning on all sex hormone merchandise to be used by biological time girls. The alleged “black box” is that the strongest step the FDA will want warn customers of potential risks from a drugs. It advises health care professionals to prescribe estrogen products at the lowest dose and for the shortest possible length of time.
While HT had conjointly till 2002 been wide accustomed forestall biological time pathology, the health risks of hormone therapy may outweigh this benefit for many women. Other osteoporosis therapies should be considered first.
Although experimental studies over a few years indicated that HT prevented cardiopathy in biological time girls, the yankee Congress of Obstetricians and Gynecologists (ACOG), the North American Menopause Society (NAMS), and several alternative skilled organizations say biological time internal secretion medical aid shouldn’t be used for primary or secondary interference of coronary cardiopathy as a result of there is not enough proof to indicate semipermanent sex hormone therapy or hormone replacement therapy improves cardiovascular outcome. However, ACOG and NAMS say girls in early change of life WHO area unit in smart vessel health might contemplate sex hormone and sex hormone for his or her biological time symptoms. Talk to your health care skilled regarding your individual risks.
Treatment
There are many formulations and dosages of estrogen and estrogen-progestin combinations on the market today for treating conditions that result from estrogen deficiency, for birth control and for regulation of hormone-related processes such as menstruation.
Hormonal contraception
Oral contraceptives
Most combination oral contraceptives contain between twenty to fifty metric weight unit of sex hormone, a lower dose (one-fourth or less) than those marketed 20 to 30 years ago.
Oral contraceptives containing estrogen are now prescribed by some health care professionals for health benefits beyond contraception. For instance, they can:
- Regulate and shorten a woman’s menstrual cycle
- Decrease severe cramping and heavy bleeding
- Reduce ovarian cancer risk
- Reduce the development of ovarian cysts
- Protect against ectopic pregnancy
- Reduce the risk of uterine (endometrial) cancer
- Decrease perimenopausal symptoms
Contraceptive patches and vaginal ring
The patch and ring contain hormones similar to oral contraceptives and provide many of the same benefits, although through a different route of administration.
Hormone-containing intrauterine device
The hormone-containing IUDs provide contraception and, in the case of the Mirena IUD, greatly reduce menstrual bleeding.
There are side effects and risks associated with estrogen-containing birth control pills, however, although many have been reduced through the introduction of lower-dosage versions in recent years. These include heart attack, stroke, blood clots, pulmonary embolism, nausea and vomiting, headaches, irregular bleeding, weight gain or weight loss, breast tenderness and increased breast size.
In addition, smoking cigarettes while taking birth control pills dramatically increases the risk of heart attack for women over 35. Smoking is way additional dangerous to a woman’s health than taking contraception pills, however the mix of pill pill use and smoking incorporates a bigger result on heart attack risk than the easy addition of the 2 factors. For women of all ages, smoking raises the risk of blood clots and stroke associated with birth control pills.
If the primary reason you are taking an oral contraceptive is to prevent unwanted pregnancy and you are worried about potential estrogen-related side effects, the “mini-pill,” which contains progestin (a synthetic form of the natural hormone progesterone), may be an option.
Hormone Therapy for Menopausal Symptoms
There are two types of therapy used to replace hormones that decline with the onset of menopause or are deficient as a result of medical conditions.
Estrogen-progestin
Postmenopausal hormone therapy, until recently referred to as “hormone replacement therapy,” or “HRT,” is now also termed “menopausal hormone therapy” (MHT) or simply “hormone therapy” (HT). HT typically refers to a combination of estrogen and either a synthetic form of the hormone progesterone (progestin) or a natural form of the hormone. Progesterone or progestin is necessary in women with an intact uterus to decrease the stimulating effect of estrogen on uterine tissue—a risk factor for uterine cancer.
Estrogen-only
“Estrogen therapy” (ET) refers to the employment of sex hormone alone. Estrogen therapy alone may be prescribed for women who have had a hysterectomy (and therefore are not at risk of uterine cancer).
A variety of estrogen medications containing various types of estrogen are available. These embody pills, patches, injections, lotions, gels, sprays, vaginal creams, rings or tablets.
Conjugated estrogens. Premarin is the most frequently prescribed conjugated estrogen therapy product. It contains many varieties of conjugated estrogens derived from the water of pregnant mares. It is available in oral, intravenous and vaginal cream formulations. Cenestin is a blend of nine plant-derived, synthetic conjugated estrogens and is FDA approved for treating menopausal symptoms.
Esterified estrogens. These estrogens may be made from plant sources or be prepared from the urine of pregnant mares. Brand names are Estratab and Menest. Estratest may be a combination of esterified estrogens and androgen, a male hormone. It is the sole androgenic hormone presently FDA approved for girls. However, oral androgenic hormone has been related to decreases in smart cholesterol, and it can cause side effects like acne and increased facial hair growth. You shouldn’t take these medications if you are pregnant or are planning a pregnancy.
Estratest. Estratest may be a combination of esterified estrogens and androgen, a male hormone. It is the only testosterone currently FDA approved for women. However, oral testosterone has been associated with decreases in good HDL cholesterol, and it can cause side effects like acne and increased facial hair growth. You shouldn’t take these medications if you are pregnant or are planning a pregnancy.
Estradiol (systemic). This type of estrogen, normally produced during the reproductive years, is available in many brand-name oral and transdermal preparations. Oral estrogen is accessible in an exceedingly range of FDA-approved brand-name merchandise, including Femtrace, Estrace, Gynodiol and generic estradiol. Transdermal patches embody Alora, Climara, Esclim, Estraderm and Vivelle. An ultra–low-dose sex hormone patch, Menostar, is approved for interference of pathology. Estradiol gel (EstroGel) is an FDA-approved bio-identical estradiol in a transdermal gel; Estrasorb is a transdermal estradiol lotion.
Estrone. This is the predominant natural hormone in menopausal women and is a product of the metabolism of estradiol. Some forms of estrone are present in conjugated and esterified estrogen preparations, as well as in combination with piperazine.
Estropipate (Ogen, Ortho-Est). This natural estrogenic substance is available in a pill.
Ethinyl estradiol (Estinyl). This synthetic estrogen is available in tablet form.
Synthetic conjugated estrogens, B (Enjuvia). This is a plant-derived, synthetic conjugated estrogen product in tablet form.
Local vaginal estrogen therapy
Several forms of estrogen are available as creams applied vaginally for treating vulvar and vaginal atrophy. They include: conjugated estrogen cream (Premarin), micronized estradiol (Estrace), and dienestrol (Ortho dienestrol).
Estradiol is also available as an inserted vaginal ring (Estring), for treating those conditions as well as urethritis, and in vaginal tablet form (Vagifem).
Combination hormone therapy: estrogen and progestin
Taking estrogen daily and progestin for two weeks every month may result in monthly bleeding similar to menstruation. Many women prefer taking both hormones every day to eliminate bleeding, which usually stops after three to six months of daily combination therapy.
Some examples of combination pills are:
- 17 beta-estradiol and norgestimate (Prefest) continuous estrogen and pulsed progesterone.
- Conjugated estrogens and medroxyprogesterone (Prempro, Premphase)
- 17 beta-estradiol and norethindrone acetate (Activella)
- Ethinyl estradiol and norethindrone acetate (Femhrt)
Some examples of combination transdermal products are:
- estradiol and norethindrone acetate patch (CombiPatch)
- estradiol and levonorgestrel patch (Climara Pro)
Any of these products may be prescribed for menopausal symptoms, including vulvar or vaginal atrophy.
Bioidentical, natural or compounded estrogen
The term “bioidentical hormones” is used to refer to hormones that are identical to the form of hormone made in the body. They may also be called “natural.” Sometimes hormones sold in a compounding pharmacy are called “natural” or “bioidentical.” All of these estrogen or progesterone products are made in a laboratory and then mixed with a cream or put into a pill form.
There is no evidence that compounded hormones are safer or more effective than FDA-approved hormones. There are many FDA-approved bioidentical estrogens and progesterones on the market and a wide range of dosing options. FDA-approved products have stricter oversight in terms of product purity and dose consistency than compounded products.
You should not take any form of estrogen if you are pregnant or have had:
- Breast, uterine or ovarian cancer
- Abnormal uterine bleeding of an unknown cause (until the cause has been determined)
- A very high triglyceride level (in this case, some women can take estrogen via a patch, lotion or gel)
- Active liver disease
- Blood clots or pulmonary embolism
Women taking either estrogen alone or estrogen plus progestin are advised to have yearly breast exams and receive annual mammograms. Potential side effects of taking ET or HT include increased risk for blood clots, heart disease, heart attacks, stroke and breast cancer (the risks of breast cancer are greater with estrogen plus progestin than with estrogen alone). Other possible side effects include:
- vaginal bleeding (starting or returning)
- breast tenderness (which often goes away after three months)
- nausea (which often goes away after your body adjusts)
- fluid retention (bloating)
- headache
- dizziness
- depression
- increased risk of ovarian cancer and gallbladder disease
- change in vision, including intolerance to contact lenses
Estrogen can interact with a variety of other commonly prescribed medications, including thyroid hormone, so be sure to tell your health care professional about all medicines you are taking, including alternative/complementary products and supplements.
In making the decision about whether to use estrogen to treat your condition, you and your health care professional will discuss your personal health history. This discussion will include considering if you are at increased risk for one or more of the conditions with which estrogen is associated.
Facts to Know
- Estrogen is produced in the ovaries, adrenal glands and fat tissues. It prepares the reproductive organs for conception and pregnancy. Estriol, a form of estrogen, is produced by the placenta during pregnancy.
- The function of estrogen in the body is complex. We have learned a lot, but there is still much more to learn.
- Declining or low levels of estrogen can cause physical symptoms including hot flashes, night sweats and vaginal dryness.
- By the time you reach menopause, you will produce only about one-third the amount of estrogen you produced during your childbearing years.
- Supplemental estrogen taken after menopause does not appear to prevent heart disease when initiated in older women several years past menopause.
- The term “hormone replacement therapy (HRT)” has been largely replaced by other names, including post-menopausal hormone therapy (PHT), hormone therapy (HT), or menopausal hormone therapy (MHT). Estrogen-alone therapy, previously referred to as estrogen replacement therapy (ERT), has been largely replaced by the term estrogen therapy (ET).
- The term “estrogen” includes a group of closely related compounds, including estradiol, estrone and estriol.
- Estrogen therapy may be prescribed for conditions such as delayed onset of puberty, genital atrophy or female hypogonadism (incomplete functioning of the ovaries, creating symptoms such as vaginal dryness, breast atrophy and lower sex drive).
- There is new evidence that long-term use of hormone therapy may increase a women’s risk of ovarian cancer and that estrogen plus progestin may possibly increase lung cancer mortality.
- Findings from a memory sub-study of the Women’s Health Initiative (WHI) indicate that women who are older than 65 when they start taking combination hormone therapy have an increased risk of developing dementia, including Alzheimer’s disease, compared with women who do not take the medication. Effects in younger women remain unknown and require further study.
Key Q&A
- The menopausal symptoms I’m experiencing since my ovaries were removed are worse than expected. Why?The abrupt decrease in hormone levels for women who have surgical menopause can cause more severe symptoms than natural menopause. Talk to your health care professional about medications and lifestyle changes that can ease those symptoms.
- Should I have my ovaries removed if I have a hysterectomy for benign disease?Increasing evidence suggests that, unless a woman is at elevated risk of ovarian or breast cancer, the benefits of keeping the ovaries may outweigh the risks. This is especially true for women who have not yet reached menopause at the time of hysterectomy. A recent study published in Obstetrics & Gynecology reported that removing both ovaries during a hysterectomy is associated with a decreased risk of ovarian and breast cancer but an increased risk of lung cancer, coronary artery disease and death from other causes, even in postmenopausal women. Talk to your health care professional about your surgical options and the best plan for you.
- I’ve heard that estrogen can affect my chances of getting osteoporosis. How?Estrogen helps reduce the rate of bone loss that occurs during normal bone remodeling. Normally there is a balance in the activity of the cells that break down bone and the cells that build it back up. By decreasing the activity of the cells that break down bone, estrogen allows the cells that build bone to have a greater overall effect. Once estrogen levels drop, this balance shifts.While hormone therapy has been shown to decrease hip and vertebral fractures, it may also increase your risk of other health conditions, such as invasive breast cancer, stroke and blood clots. Discuss the risks and benefits of available treatments with your health care professional.
- What sort of side effects can I expect when taking estrogen?The most common side effects are breast tenderness, water retention and uterine bleeding.
- How does hormone therapy affect breast cancer risk?According to the American Cancer Society, taking estrogen alone is not linked to a higher risk of breast cancer. In fact, in certain groups of women, such as those with no family history of breast cancer or no personal history of benign breast disease, estrogen may lead to a slightly lower risk of breast cancer.The story is a little different for women taking a combination of estrogen and progestin, however. The Women’s Health Initiative found taking estrogen and progestin replacement therapy was linked to a higher risk of breast cancer. Specifically, for every 10,000 women who took estrogen and progestin hormone replacement therapy each year, there were eight more cases of breast cancers than there were in women who hadn’t taken the hormones. And the longer a woman took estrogen and progestin replacement, the higher her risk. However, this risk drops within three years of stopping the hormones but remains slightly elevated compared to women who never used combination hormone therapy. The ACS also reports breast cancers in women taking estrogen and progestin replacement therapy tend to be larger and possibly more advanced once they are found.HT can also increase breast density and make mammograms less reliable.
- How does estrogen affect cardiovascular health?ACOG and NAMS say menopausal hormone therapy should not be used for the primary or secondary prevention of heart disease because there isn’t enough evidence to show long-term estrogen or estrogen plus progestin therapy improves cardiovascular outcomes. However, ACOG says women in early menopause who are in good cardiovascular health may consider estrogen plus progestin for menopausal symptoms. Talk to your doctor about your individual risk.
- What is known about the benefits of hormone therapy on bone health?Postmenopausal osteoporosis is characterized by decreased bone mass, deterioration of bone architecture and high bone fragility, making bone fractures of great concern. Estrogen deficiency is the most common risk factor for osteoporosis in women.
Estrogen, with and without progestin, has been shown to be a protective and effective prevention measure against osteoporosis and the risk of clinical fractures. However, considering the potential risks of HT uncovered in the WHI, such as increased risk of cardiovascular disease and breast cancer, it is no longer recommended as a first-line therapy for osteoporosis.
Other ways to reduce the risk of osteoporosis include avoiding tobacco, increasing weight-bearing exercise and resistance training and having adequate intake of calcium and vitamin D.



